Then of course, there is the relatively new research which suggests that menopause depression also impacts stress eating and weight gain. I know in a really tough past-year for everyone, it’s hard to differentiate your worsening moods and melancholy from being in lockdown, especially those of you in Australia and here in New Zealand.
But if you are also in menopause (your periods have stopped) or post-menopause (they’ve stopped for a year or more), please don’t blame both depression and weight gain entirely on lockdown. Because menopause hormonal changes and depression may be having an effect on your eating behaviour too.
That’s why the article from Schrieher and Dautovich fascinated me. I read it after wondering why on earth I felt so depressed as I arrived in my 50’s. The researchers called the menopause transition a “window of vulnerability” for the development of depressive symptoms given the changes in hormonal levels (Schreiber & Dautovich, 2017) and due to feeling depressed, we also run the risk of over-eating in order to ‘cope’. Sound familiar?
As such, we may also head towards weight gain and worsening health as we age. Then becoming overweight cause our hot flushes to ramp-up in frequency and severity. For some of you, this is despite your anti-depressant therapy.
Psycho-social factors such as ‘stress-eating’ play an important role in the association between depressive symptoms and weight, state Schrieber and Dotavich (2017) in their research on menopause-related depressive symptoms and weight gain.
The results highlight the need to focus on both behavioural factors as well as menopausal status when working to resolve our symptoms. Knowing this connection is important – as it was for me as well.

Feeling depressed or experiencing frequent mood swings in peri-menopause and menopause is all about the connection between all of your hormones – not just oestrogen, progesterone and serotonin – which is why I’m sharing my own discoveries from the research about depression with you in this article. Many of us have very little understanding of what’s going on at this time of our lives.
Menopause depression is due to lowering serotonin. This is your mood hormone. If you’re feeling stressed and over-whelmed with all that’s going on in your life and you are in your menopause transition, then the decline in oestrogen also has an effect on your brain hormone, called SEROTONIN. When oestrogen is lowering in menopause, serotonin follows it on a downward slide.
Serotonin is your mood-boosting hormone and its decline during menopause, can make you feel depressed. Some of you on anti-depressants will already know this,, but what you may not know is that menopause depression is linked to the build-up of inflammation in your body.
Ageing itself is inflammatory.
I’ve talked about the new research on ‘inflammaging’ in other posts, so look for these on my website when you can. Inflammation arrives in mid-life, not only due to our changing cells and tissues, but also to the fact that we aren’t sleeping or our nutrition isn’t meeting our needs or because we are doing lots of exercise, or we feel stressed, or we are experiencing lots of hot flushes (a catch-22, if you are overweight).
Inflammation comes from numerous sources and it’s good to explore what these sources may be for you.
For example, when Hot Flushes are more than 5 an hour, our body overheats and becomes inflamed. This inflammation then causes an acceleration in the decline of SEROTONIN.
But there’s other factors contributing to menopause depression too.
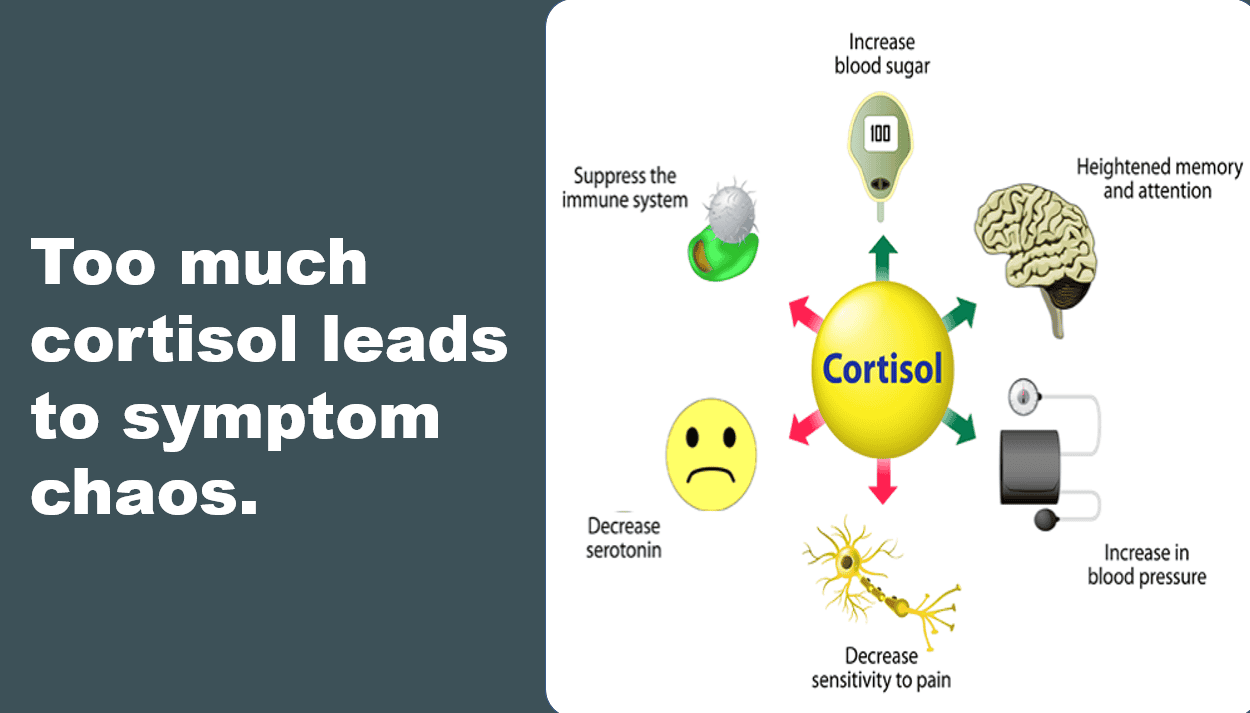
- High cortisol is linked to depression, so too is insomnia. If you aren’t sleeping and you are feeling stressed, then you may be producing too much of your chronic hormone, Cortisol. Higher than normal levels throughout the day causes more inflammation in organs, muscles and blood vessels as we biologically age. The accumulation of high levels of cortisol, can disrupt serotonin production more rapidly during menopause. The result? More depression and weight gain.
- Your gut and liver health also matter – not only to your feelings of depression but to your urges to ‘stress-eat’ as the research I mentioned above indicates. When liver inflammation is present in cells and tissues or if women are putting on belly fat and have poor gut health or eating a high fat diet, then B vitamins may not be absorbed and metabolised very well and B-vitamins are important for managing menopause depression.
- Low Vitamin B6 and B12 increase depressive episodes (Feraj, 2017). This is why for women who want to improve their moods and motivation during menopause, it’s important to turn around liver and gut health first, especially for women who are overweight.
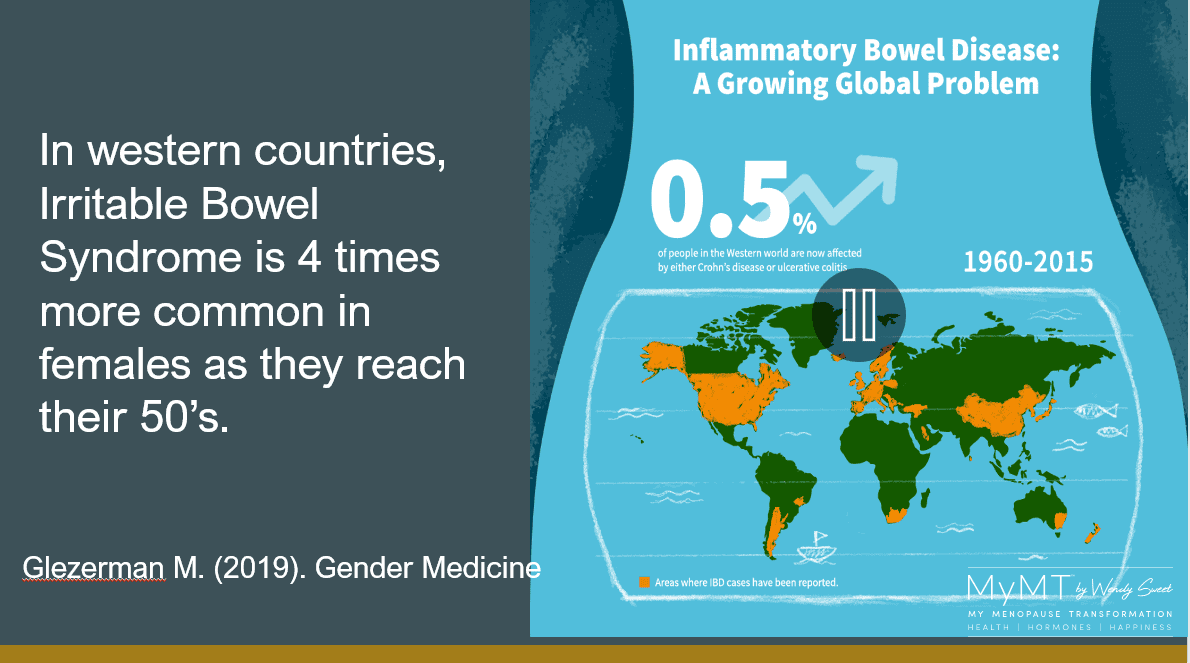
The gut-brain connection scientific evidence is increasing in relevance for women in their menopause transition. Over the decades gut health may have changed and too often women develop Irritable Bowel Syndrome (IBS) or Diverticulitis when they reach their 50’s. Researchers now understand that the powerful connection between our immune system and our gut has a profound effect on our mental health if our gut health is impaired. This is because gut inflammation impacts on the absorption of a protein called Tryptophan, which helps to make serotonin.
3 Changes to Make to your Lifestyle if you Feel Depressed
(1) Adjust the type, timing and amount of your food intake. We are the generation of dieters, especially low carb diets. But these do not work during menopause when it comes to our moods. When we don’t eat regularly or we don’t eat the right carbohydrates (especially if we are exercising), this affects your insulin production and blood sugar levels.
When blood sugar levels are low, your pancreas secretes a hormone called glucagon to re-set your blood sugar levels. Eat too much and your pancreas releases insulin to help regulate your blood sugar levels. When both glucagon and insulin are un-balanced, our mood swings and feelings of depression occur because there is a powerful link between your blood sugar hormones and serotonin production.

(2) Focus on restoring your sleep patterns and reducing your hot flush frequency. Poor sleep means that your adrenal glands (which produce your ‘fight or flight’ hormones) become overwhelmed and this impacts on your thyroid function. Low thyroid response results in low energy levels and even more stress on your adrenals. When we are feeling stressed or we have oxidative stress from inflammation in our tissues, our sleep suffers, we get more hot flushes and our mood swings become worse. This is why turning around your circadian rhythm matters more for your weight loss in menopause than any crazy diet you might be on.

(3) Ask for your Vitamin D levels to be checked. Especially if you live in the Northern Hemisphere at the moment. Low Vitamin D3, depression and worsening inflammation go hand-in-hand. Vitamin D is often low in menopausal women because it decreases with changes to oestrogen receptors in our skin. (Lerchbaum, 2013).
I talk a lot about Vitamin D and this connection with menopause with women, because so many of us work inside and if women have darker skin, then their Vitamin D absorption is lower too. If women are also overweight and carrying more belly fat, then because Vitamin D is drawn to fat in fat storage areas, the Vitamin D can go to adipose tissue and not to where it is needed – in muscles, bones, nerves and the heart. [Dregan, Rayner, et al., 2020).

In the two to eight year period known as ‘peri-menopause’ the production of oestrogen is declining. Because oestrogen is a hormone, when levels reduce it affects the function of not only progesterone, but other hormones in the body as well, including your mood hormone serotonin. When serotonin levels are low, this impacts on other hormones produced by your thyroid, adrenal and more importantly, your pituitary glands where serotonin production occurs.
Depression that arrives during menopause is frightening – especially if you have never experienced it before. You should therefore, always follow up with your Doctor, as well as explore lifestyle solutions that will help you manage it as well.
These specific lifestyle solutions are what women on the 12 week MyMT™ programmes discover, no matter whether you are on supplements, HRT, bio-identical hormones or medications such as anti-depressants either.
Because when you understand what to do and why, like Brenda above beaming at you from the beautiful Tasmania, you will feel so much better too.
Wendy

References:
Doyne, E. et al. (1983). Aerobic exercise as treatment for depression in women. Behavior Therapy, 14(3), 434 – 440.
Dregan, A., Rayner, L., Davis, K., Bakolis, I., Arias de la Torre, J., Das-Munshi, J., Hatch, S. L., Stewart, R., & Hotopf, M. (2020). Associations Between Depression, Arterial Stiffness, and Metabolic Syndrome Among Adults in the UK Biobank Population Study: A Mediation Analysis. JAMA psychiatry, 77(6), 1–9. Advance online publication.
Feraj, J. (2017). Micro-nutrients, depression and inflammation among women of reproductive age. Doctoral Dissertation 993, University of Massachusetts.
Lerchbaum, E. (2014). Vitamin D and menopause – A narrative review. Maturitas Journal, 79, 3-7
Schreiber, D, & Dautovich, N. (2017). Depressive symptoms and weight in midlife women: the role of stress eating and menopause status. Menopause (New York, N.Y.), 24(10), 1190–1199.
Vivian-Taylor & Hickey, M. (2014). Menopause and depression: Is there a link? Maturitas Journal, 79, 142-146

