It’s the dipping that you need overnight. Generally it occurs between 2-4 am – just that time of night, that you may be lying awake, your partner is snoring and you are worrying about well, … everything really. Maybe you are even getting up to use the bathroom – afterall, since you’ve been in menopause, the nightly trips to the bathroom may have increased!
So, I’ll break the bad news to you first. The longer you go without sleeping all night, the worse your blood pressure may become, your weight might climb and you not only feel exhausted, but your blood vessels age more rapidly too.
I used to worry about all these things myself, especially the changes to my cardiac health and weight.
Before the pandemic I met a lady at one of my seminars who told me that she was reading a book about sleep and the advice was to get up and ‘do something’. So, she was getting up around 3am, making a cup of tea and doing her ironing for an hour or so whilst watching TV. I’ve read this type of advice too, but I disagree.
There’s a reason I disagree with women getting up in the night and that is to do with their unique hormonal changes in menopause and the effect that this has on their blood pressure overnight. Insomnia, followed by activiy and of course, watching television increases our stress hormone called cortisol and this elevates blood pressure.
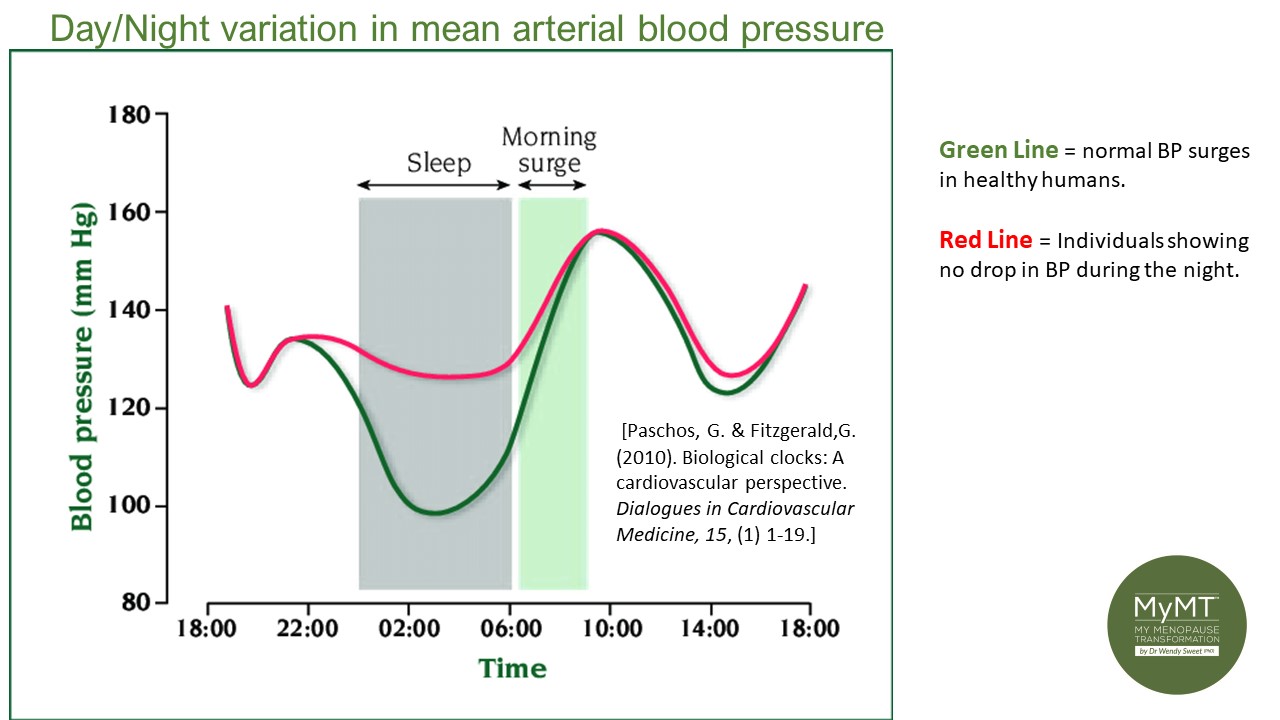
If women aren’t sleeping, then they make be experiencing the phenomenon of ‘non-dipping’ of their blood pressure. This can lead to higher blood pressure as we age.
When my menopause hormonal changes robbed me of my precious sleep, I used to get up in the night too. Invariably this was to use the bathroom, but sometimes I did some work. But I now better understand that this was the wrong thing to do …. because my blood pressure would remain higher overnight. It wouldn’t ‘dip’ down, which is what is supposed to happen.
In the United States, the highest rates of menopause-related insomnia complaints are among post-menopausal women at 43%–48% (Drake et al, 2019). Goodness knows what this rate is globally.
The report goes on to mention that menopause itself—via hormonal changes and related symptoms – often leads to sleep deterioration, thereby triggering the onset of insomnia disorders which of course, leads to higher blood pressure (hypertension), weight gain, depression and other diseases of ageing which relate to inflammatory changes.
This is why I always say that if we are going to get serious about improving our symptoms as well as our health as we age, turning around menopause-related insomnia is crucial.
Whilst there are numerous causes of high blood pressure and changing heart health in our menopause transition, one of the factors that we have to take seriously is our menopause-insomnia. Not only has this got to do with our changing hormonal status as we age, but it’s also to do with whether you are an overnight ‘non-dipper’ or not. It’s why I always support getting your blood pressure checked as you transition menopause. It’s important to our cardiac health to understand what it’s doing – not only over the course of the day, but overnight too.
What is Overnight non-dipping Blood Pressure?
First described in 1988, the night time dip has become an accepted measure of cardiovascular risk. The ‘dip’ is defined as the difference between the mean systolic pressure in the day and mean systolic pressure during the night.
Over the years, research has shown that poor sleep quality, sleep curtailment, and sleep disorders (e.g., sleep apnea) are linked with BP ‘non-dipping’ overnight and a surge in blood pressure in the morning – if you are getting extreme hot flushes in the morning when you wale up, then you might want to talk to your Doctor about getting your blood pressure checked.
When this non-dipping happens and we experience insomnia, researchers have found that there is a chain of events that may lead to chronic hypertension (high blood pressure). These events include:
- Higher activation of our nervous system (a higher arousal state whereby we worry more and become anxious – often the cause of not being able to get to sleep).
- Changes to our kidney function and sodium retention (often leading to bloating and puffiness in menopausal women).
- Changes to our immune system (leading to conditions such as fibromyalgia)
- Changes to the pituitary-thyroid-adrenal axis (HPA-axis) – this can lead to worsening sleep patterns and thyroid problems. When both our sleep and thyroid function is affected, our temperature regulation is too. Hot flushes and night-time sweats are managed with sleep and a focus on reducing your blood pressure.
Turning around your Menopause Insomnia needs a focus on Managing Blood Pressure
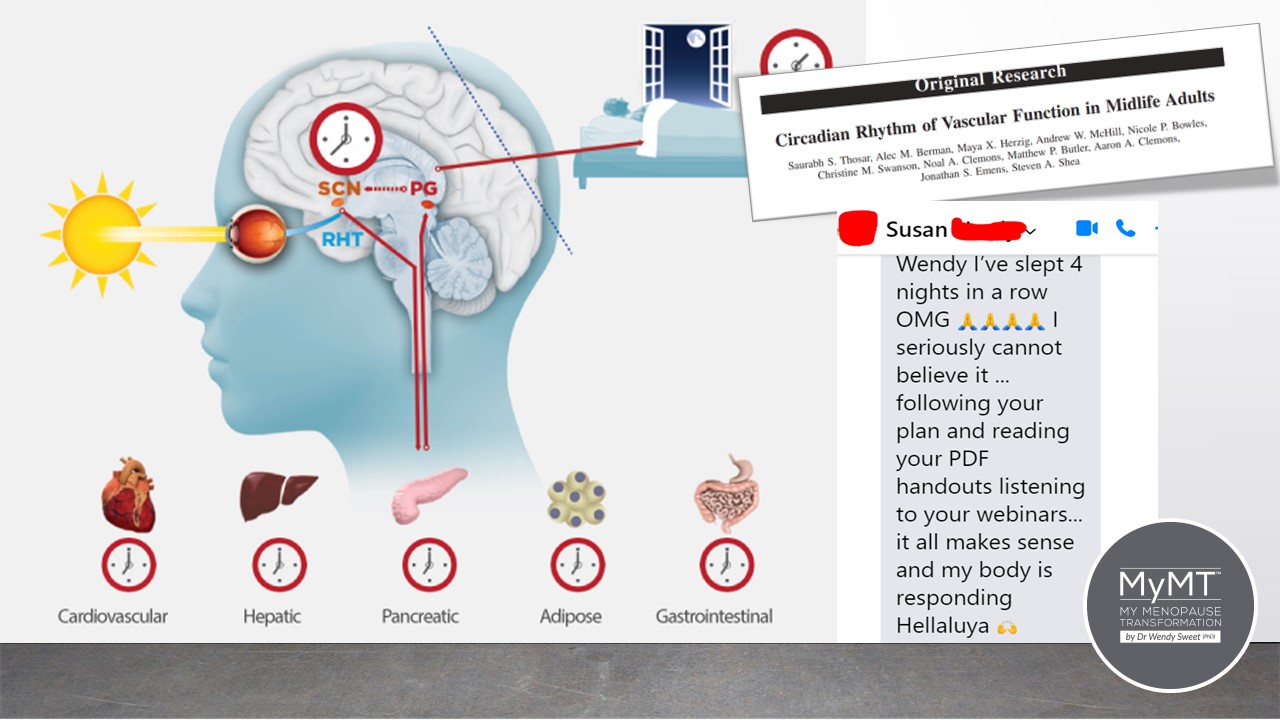
It has been well established that sleep patterns follow a circadian cycle. But so too does your blood pressure and blood vessel changes. The circadian cycle is also impacted by food and metabolic signals and I have an emphasis on the timing of eating dinner in my Sleep All Night module in both of the MyMT™ porgrammes – especially for those of you doing shift work.
Eating 3-4 hours before bedtime is important to help to reset your circadian clock as is maintaining a lower blood pressure before bedtime.
With my focus on post-menopause women this month, blood pressure management is an important topic. Other factors also affect blood pressure too, as some of you will already know.
For example, the role of salt in blood pressure management as we age is another factor for you to consider. Reducing the amount of salt you have on your meal at dinner is important – table salt is high in sodium and increases blood pressure and you don’t want to go to bed with higher blood pressure, so thinking about your sodium intake in the evening can help you.
Eating more fruits and vegetables also help your blood pressure, because you will be increasing your intake of potassium-rich foods.

Do you rest before bedtime?
Midlife is a pivotal stage in the life-course of women and this is because our hormonal changes during menopause impact other structures around the body, including in the heart and cardiovascular system.
Hence, reducing your activity before going to bed is another strategy to help you to lower your blood pressure at the end of the day. If you’ve been busy all day, or exercising or you are in a physically active job, then put your feet up at the end of the day. This improves venous return of blood in your lower legs back to your heart. Just this simple action helps to improve your blood pressure.
A heavy workout or weight training can also keep blood pressure elevated for hours – if your blood pressure doesn’t return to normal resting levels, at least 2-3 hours after heavy exercise, then please get it checked out by your Doctor. I’ve come across numerous mid-life Personal Trainers, Exercise Instructors and gym-members who are racing to the gym after dinner to do more vigorous exercise, thinking that it is ‘good for them’. Then they complain that they aren’t sleeping. Yes, the two issues are related!
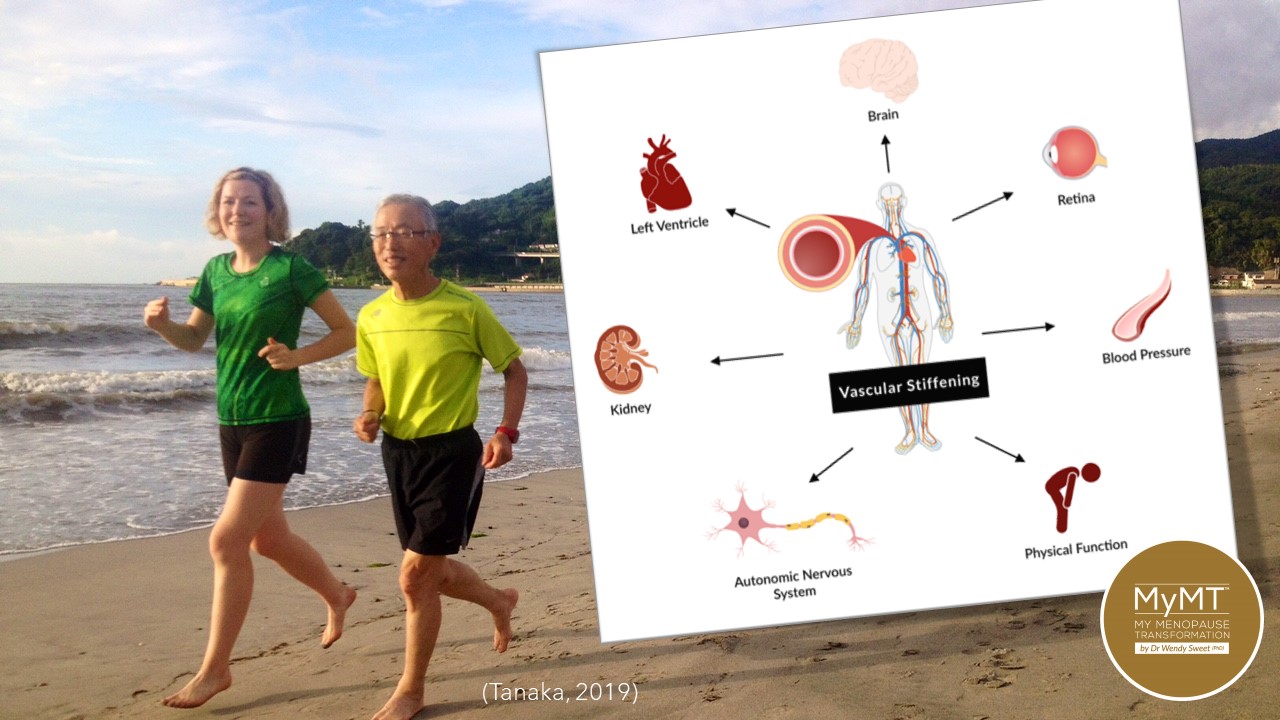
As women transition menopause, blood vessels lose elasticity and acquire inflammatory changes. Hence, it’s no surprise to me that the American College of Sports Medicine (2004) recommends exercise programmes that primarily involve endurance activity to prevent the development of hypertension and to lower blood pressure.
I’ve written a lot about how we need to implement lifestyle strategies to reduce stiffness of our blood vessels as we age – and I talk about this in my 12 week online Rebuild My Fitness programme, which numerous women do after one of the other foundation programmes (read about these HERE).
We must remember that our menopause transition opens the door to our Blood Pressure changes because we are ageing. This is natural. However, we become more vulnerable to cardiovascular changes with age, because our arteries (and lymphatic vessels) are losing the role of oestrogen, which in the past has kept our blood vessels elastic. Hence, we need to adjust our lifestyle to accommodate these changes. Lifestyle modifications are advocated for the prevention, treatment, and control of hypertension with exercise being an integral component.
Exercise programs that primarily involve endurance activity prevent the development of Hypertension in adult women with both normal blood pressure and those with hypertension. The Blood Pressure lowering effects of exercise are most pronounced with those who engage in endurance exercise at least 3-4 times a week, but again, if your joints are sore, or you aren’t sleeping or you are overweight, then as I mention to women who join me on my 12 week programmes, you need to address these other issues first.
Insomnia and the subsequent effect on blood pressure is endemic to women transitioning through menopause. But it doesn’t have to be.
Un-raveling the science of not sleeping as we transition into our new hormonal environment in menopause took me hundreds of hours of study. But I was so determined to understand why I wasn’t sleeping, because I knew from the emerging cardiovascular science, that sleep and hypertension go hand in hand.
Not sleeping leads to ongoing inflammation in our muscles, joints, liver, gut and heart. What’s more, the increasing inflammation can send us into the cascade of chronic health changes that hit us in our post-menopause years, including auto-immune health problems.
In women, vascular ageing appears to be accelerated during the menopause transition, particularly around the late perimenopausal period, presumably
related to declines in ovarian function and oestrogen levels.
Many women go on HRT which helps them enormously (and I don’t interfere in any medications women are on, because this is between you and your Doctor), but I am passionate about you understanding the lifestyle-science solutions that you can put into place too.
The term ‘Circadian’ means “about a day.” This internal clock, which gradually becomes established during the first months of life, controls the daily ups and downs of biological patterns, including body temperature, blood pressure, and the release of hormones. Circadian rhythms make people’s desire for sleep strongest between midnight and dawn, and to a lesser extent in mid-afternoon.
Our changing menopause hormones cause disruption to our normal circadian rhythms and this affects the stiffness in our blood vessels too because the cardiovascular system has a strong circadian rhythm: blood pressure should be lowest when we are sleeping but it rises sharply upon waking up.
These circadian variations are important to our health as we age, so as we transition into or through menopause, then it’s really important to restore this biological rhythm and make adjustments to get us back sleeping all night. Whilst a lot of information about sleep has emerged recently, much of this is not focused on mid-life women specifically nor on the specific gut hormones that also become affected in menopause.
If we don’t turn around our sleep in mid-life, then I’m always telling women, that this will then become their ‘new normal’, because over time, our brain and body start to read this 3am ‘awake’ period as routine.
When you aren’t sleeping, then this quickly becomes your ‘new normal’ and it can then go on for years. Over time you may accumulate more fatigue, muscle soreness, headaches, weight gain and more. That’s because your Circadian Rhythm affects nearly every organ in your body.
Dr Wendy Sweet, (PhD) Member: Australasian Soceity of Lifestyle Medicine & Founder of MyMT™
PS: If you are in post-menopause then don’t forget to check your emails from me for my July post-menopause weight loss special. Women are already underway and loving what they are learning.
References:
American College of Sports Medicine (2004). Exercise and Hypertension Position Stand. Medicine & Science in Sports & Exercise, 0195-9131/04/3603-0533
Bloomfield, D., & Park, A. (2015). Night time blood pressure dip. World Journal of Cardiology, 7(7), 373–376. https://doi.org/10.4330/wjc.v7.i7.373
Carr, M. (2003). The Emergence of the Metabolic Syndrome with Menopause. The Journal of Clinical Endocrinology & Metabolism 88(6):2404–2411
Calhoun, D. A., & Harding, S. M. (2010). Sleep and hypertension. Chest, 138(2), 434–443.
Davis, S., Castelo-Branco, C. et.al. (2012). Understanding weight gain at menopause. Climacteric, 15: 419–429.
Harvard Health Report (2017). Improving Sleep. Harvard Health Publication.
Geddes, L. (2019). Chasing the Sun: The new science of sunlight and how it shapes our bodies and minds. London: Profile Books.
Jarrin D., Alvaro P., Bouchard M., Jarrin S., Drake C., Morin C. (2018). Insomnia and hypertension: A systematic review. Sleep Med Rev. 41:3-38.
Moreau, K. L., & Hildreth, K. L. (2014). Vascular aging across the menopause transition in healthy women. Advances in vascular medicine, 2014.
Nyberg, S., Singh-Manoux, A., Pentii, J. et al. (2020). Association of healthy lifestyle with years lived without major chronic diseases. JAMA Inernal Medicine Online.
Reinke H. & Asher G. (2017). Circadian clock control of liver metabolic functions. Gastroenterology, 150: 574–580.
Rizzi, M. et al. (2016). Sleep Disorders in Fibromyalgia Syndrome. Journal of Pain Relief, 5:2, 1-5
Sharma, S. & Kavuru, M. (2010). Sleep and Metabolism: An Overview. Int. Journal of Endocrinology, Article ID 270832, 1-12.
Tanaka, H. (2019). Antiaging Effects of Aerobic Exercise on Systemic Arteries. Hypertension, 74: 237–243
Woods, N. et al. (2009). Cortisol Levels during the Menopausal Transition and Early Postmenopause: Observations from the Seattle Midlife Women’s Health Study. Menopause, 16(4): 708–718.
Yano, Y., Kario, K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertens Res 35, 695–701 (2012). https://doi.org/10.1038/hr.2012.26
Related Tag: Menopause Supplements NZ


