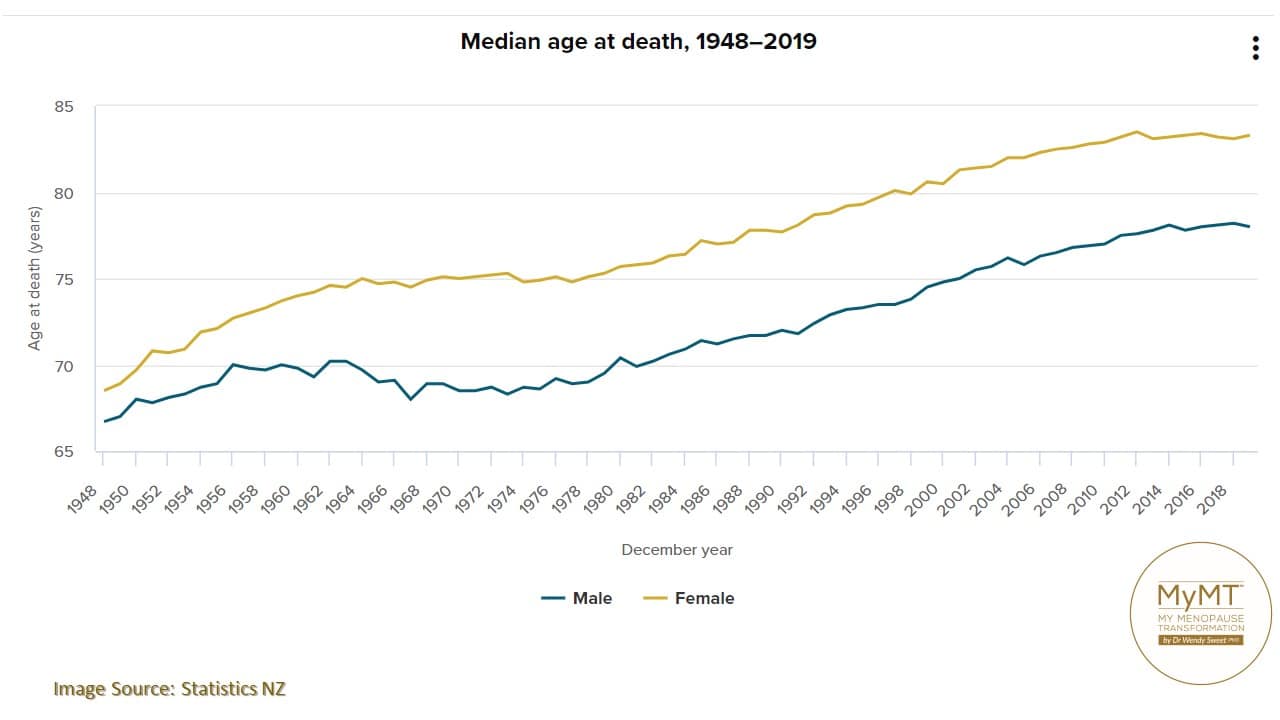
Women dying at the end of World War 2 in New Zealand, didn’t have to worry too much about menopause affecting how they were ageing did they? As you can see from the Statistics New Zealand graph below, the average age of death was under 70 years old.
Interestingly, it was heart disease (which causes angina, heart attacks and heart failure), and influenza that led many to an early death.
A similar outcome today in the context that heart disease in women aged 50 and over, resulted in more deaths from the 1990s, among New Zealand women than any other single cause. In the 2000s the rate of heart disease among New Zealand women was higher than that among women in Australia, the United States, and Canada. (Statistics NZ).
Back in the late 1940s and early 1950s, very little was known about the effects that menopause had on our cardiovascular health. Fortunately today, this is changing – mainly due to research on ageing specific to women.
Since life-expectancies have been improving steadily in many western countries, research on ageing has been gathering momentum over the past decade. I’m pleased that it has.
You see, how well women are ageing matters and ‘how’ we are ageing, starts in our menopause transition, which is the gateway to our biological ageing. Immune dysfunction and changes in inflammatory pathways are known contributors to the ageing process and tissue deterioration.
For health practitioners who join me on the Practitioner CPD/CEU 12 week programme, I talk a lot about ageing and draw their attention to the women’s health and ageing research. Positioning the peri-menopause to post-menopause transition in the ageing science matters and this is the position I take in the MyMT™ symptom reduction and weight loss programmes.
The Rise of Chronic Inflammation in Midlife:
Declining oestrogen and progesterone as well as the decline of our master pituitary hormones that control reproduction, causes changes to our immune system, lungs, heart, muscles, nerves and blood vessels. Many of these changes cause a chronic inflammation, especially if women aren’t sleeping.
Longevity researchers who study ageing and health have contributed huge amounts of knowledge to the understanding of ‘how’ we age.
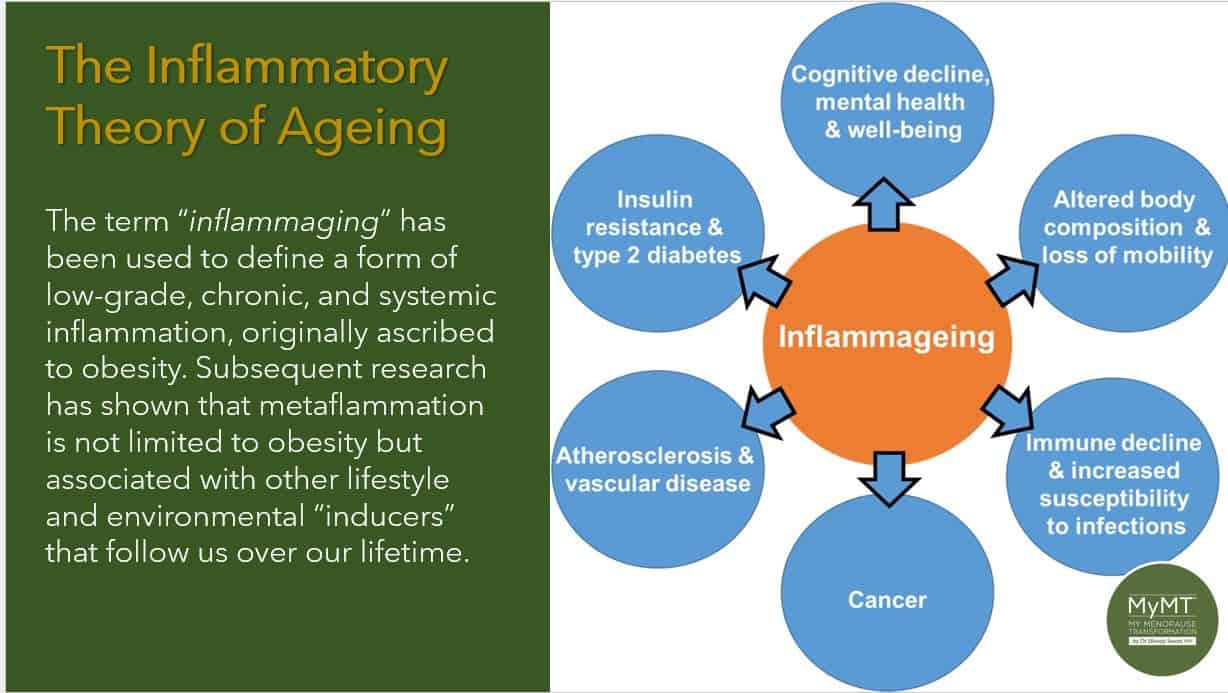
One of these researchers is Australian, Professor Garry Egger, who is known around the world as one of the pioneers of Lifestyle Medicine. I first heard Professor Egger at a health and ageing conference in Australia when doing my PhD. I was fascinated with his insights into the powerful connection between our health, inflammation and ageing. It was from him, that I first heard the term ‘Inflammaging’.
Suddenly my aching knees, sore muscles, changing gut health, mood swings and weight gain during my menopause transition, began to make a whole lot of sense.
It was the first time that I began to look at our menopause symptoms through the lens of health and ageing research. The research from Professor Egger and others has been life-changing for thousands of women on my programmes who are now heading into post-menopause and wanting to turn around their health as they age.
As Practitioners also progress through their CPD Course, they learn about factors that contribute to inflammation as women age (factors that are pro-inflammatory, and most importantly, factors that are anti-inflammatory). This is not ‘just’ about food either. It’s about sleep, energy, gut health, joint health as well as exercise that is helpful, not harmful.

The central issue in ‘inflammaging’ is that as we move through our 50s and beyond, our cells and tissues are undergoing changes that whilst part of our natural life-cycle, are also caused by the life-long exposures that our immune system has had to environmental and stress-related stimuli.
From an evolutionary perspective, a variety of stimuli keep us in the ‘inflammaging’ cycle and I include menopause-related hormone changes in this too. As Professor Egger stated, “We have been operating in silo’s. We haven’t been taking into account all the other effects on inflammation, including ageing and for women, hormonal changes too.”
Many of these effects stem from changes to our food production, e.g. chemical exposure, changes to our exercise patterns, e.g. too much or not enough exercise over the years, changes to our sleep patterns and of course, changes to our stress levels. These are all factors which affect women as they transition through menopause.

Understanding the role of ‘inflammaging’ in the life-course of chronic disease, fuctional decline and frailty across the lifecourse has led researchers to focus on our immune system.
For women in menopause and going into post-menopause, when periods have ended for a year or more, there is a greater susceptibility to the occurence of this low-grade chronic inflammation, that is now seen as contributing to post-menopause heart disease, auto-immune problems such as fibro-myalgia, and increased vulnerability to infectious disease. (Baylis, Bartlett et al, 2013).
Whilst there is now convincing evidence that how rapidly we ‘age’ is connected to our genetic pre-disposition, there are other contribitors to our ageing that hasten this accummulation of inflammation. I talk about these in my 2 hour Masterclass on Menopause webinar which is now online for you, but some of these pro-inflammatory factors include:
- Exposure to life-long stressors that in women, affects the accumulation of our chronic stress hormone called, cortisol.
- Damage to our DNA, in particular the telomeres which are the protein complexes that protect our DNA.
- A modern, western diet, full of processed foods, fats and sugar.
- Poor gut microbiome health.
- Inadequate sleep which prevents the immune system from healing and repairing overnight.
- Being overweight or obese.
- A high alcohol intake.
- Smoking.
- Stress.
Sorting out Sleep Improves Symptoms and Heart Health
When we all lead such busy lives, it’s so important to get our sleep sorted as we move through menopause and into post-menopause. I can’t reiterate this enough.
As I often mention to women on my programmes, when we have been waking up night after night, then our brain and body reads this as our ‘new normal’ and we keep waking up. But this is what leads us down the path towards worsening inflammation in our cells and tissues as we age and worsening cardiovascular health.
Not sleeping is now recognised as one of the main contributing factors to changing health as we move into our post-menopause years, and a factor in post-menopause heart disease as well. The United Kingdom, Australia and New Zealand have some of the highest incidence of post-menopause heart disease in the western world.
If we aren’t sleeping, our heart and immune system stay under stress all day long, particularly, when we are regular exercisers or we have busy, stressful jobs or home environments. That’s why I love getting women sleeping all night. It helps to reduce their worsening symptoms in menopause. And yes, your diet is important in turning around symptoms too, but sleeping all night, to me, rates more highly because the human immune system and sleep are both associated and influenced by each other. And because
Our immune system is under programmed senescence. This is the term which describes programmed biological ageing. Think of autumn leaves discolouring and falling from a tree. This is an example of programmed senescence in plants. Because we are ageing, our immune system is as well. As such, it doesn’t produce as many immune-fighting lymphocyte cells in our bone marrow. When we don’t sleep, we are behind the eight-ball with our immune health even more.
Sleep deprivation makes a living body susceptible to many infectious agents too – a concern for all of us within the context of the current state of the world at the moment.
Sleep deprivation was so frustrating for me as I know it will be for many of you. I knew that my body wasn’t healing and recovering overnight and not sleeping was leaving me too exhausted to recover from the exercise I love to do.
At the time, I also didn’t understand that not sleeping was blocking fat-loss mechanisms overnight and causing increased hot flushes because blood pressure and cortisol remain higher during the day when we don’t sleep. Cortisol that does not follow the normal daily diurnal sleep/ wake pattern can trigger blood sugar imbalances, food cravings and fat storage, especially around the middle.
As we move into menopause, cortisol needs to be settled down, especially in the context of inflammaging and heart health and we need to understand that as our periods end, our need for iron changes as well. High iron levels are now known to impact post-menopause heart disease as women transition through menopause.

But back to cortisol.
It’s one of our chronic stress hormones and it’s important to women in menopause who aren’t sleeping, because it works in synergy or partnership with our sleep hormone melatonin. If cortisol levels are too high when we go to bed, then we don’t produce enough melatonin to keep us asleep for the healing hours between 2-4am.
Then if melatonin levels are lower than normal, we either can’t get off to sleep or we wake up in the night or we don’t sleep deeply enough to have the restorative sleep that we so need to keep our energy levels up for all that we do in our day.
“Our capacity to remain healthy is badly affected by loss of sleep and sense of comfort” reports researchers who have looked at the role of sleep on the immune system.
They go on to state that our white blood cells, called leukocytes, don’t reach the levels that they should due to lack of sleep and this makes us vulnerable to sickness, flu and immune system health changes. For women in menopause, this may also lead to the autoimmune problem of fibromyalgia.
When we don’t sleep and our sleep-wake cycle is affected, then our nervous system is also affected leaving us feeling more anxious and ‘wired’.
Overnight our nervous system and immune system work together – this is why when women are going through menopause and are waking up night after night, they feel wired, they feel hotter than normal and their muscles and joints remain sore or they put on weight. In other words they remain ‘inflamed’ but many, like Sharon, in Australia, become frustrated when exercise doesn’t help them to lose weight but leaves them injured instead.
The good news is that in more recent years, scientists such as Professor Egger have opened the door on the positive changes that we can make to our daily lifestyle to reduce the speed of inflammaging. It is becoming known that the progression of many chronic diseases can be slowed or even reversed.
Scientists are also gaining new insights into how exercise may be an effective strategy to mitigate the effects of inflammaging and in the MyMT™ programmes
I get women off exhausting high intensity exercise, until they are sleeping all night. This aspect, for numerous women is the main contribution to their frustration with exercise not helping them to lose weight! It was the same for me as well as numerous women I interiewed as part of my doctoral studies.

For women coming to join me on the online MyMT™ programmes, I coach them how to manage their inflammaging. That’s because I’ve positioned our menopause transition in women’s ageing science. The strategies to sleep all night are fundamental to this as is improving cardiac, liver, gut and joint health.
As well, the dietary approach I use focuses on specific nutrients that help to reduce inflammation in our body as we age. This includes foods such as citrus fruits, beets and celery, all of which are evidenced to help improve blood pressure and blood vessel dilation.
With over 5000 women now having gone through this online lifestyle-change programme in over 50 countries, it would be my privilege to support and guide you. If you are thinner or leaner, then the Circuit Breaker programme is for you, otherwise the weight loss Transform Me programme is the one to choose.
If you would like to know how the programmes work, then you can read about this HERE. I hope you can join me and if you are a Health Practitioner, then please sign up to my weekly newsletter HERE. This is designed to give you the evidenced information you need to help your clients!
Dr Wendy Sweet (PhD), MyMT™ Founder and Member: Australasian Society of Lifestyle Medicine.

References:
Asif N., Iqbal R., et. Al. (2017). Human immune system during sleep. American J. Clin Exp Immunol.,6 (6):92-96
Baylis, D., Bartlett, D.B., Patel, H.P. et al. (2013). Understanding how we age: insights into inflammaging. Longev Healthspan 2, 8. https://doi.org/10.1186/2046-2395-2-8
Egger, G. & Dixon, J. (2009). Obesity and chronic disease: always offender or often just accomplice. British Journal of Nutrition, 102, 1238-1242.
Ferrucci L. & Fabbri, E. (2018). Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 15(9):505-522. doi: 10.1038/s41569-018-0064-2. PMID: 30065258; PMCID: PMC6146930.
Franceschi, C. et al. (2018) Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat. Rev Endocrinology, 14(10):576-590.
Lee, E., Anselmo, M, Tahsin, T. et al. Vasomotor symptoms of menopause, autonomic dysfunction, and cardiovascular disease. 2022, Am. J. of Physiology,
McCarthy M, Raval AP. The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. J Neuroinflammation. 2020 Oct 23;17(1):317.
Neves J., & Sousa-Victor, P. (2020). Regulation of inflammation as an anti-aging intervention. FEBS J. 287(1):43-52. doi: 10.1111/febs.15061. PMID: 31529582.
North American Menopause Society (12th Oct. 2022). Hot flashes are not just uncomfortable but also could be hard on the heart.
Theurey, P. & Pizzo, P. (2018). The Aging Mitochondria. Genes, 9(22), 1-13. doi:10.3390/genes9010022

