Every week in my newsletters I try to come up with a topic that I hope will interest you. Sometimes it’s because of a conversation in my coaching group from other women who are just like you, or sometimes I’m reminded of something that I had no idea was anything to do with our menopause transition because nobody mentioned it to me when I sought help with my symptoms.
The conversation about menopause supplements that are heavily marketed to women and come out of America. I explained that I always look at the ingredients to better understand what are the main compounds and what they do.
When I googled the ingredients in these supplements, they were all ingredients that are used in gut health repair – not one ingredient was to do with menopause … but then again, one could argue that they actually were.
Did you know that gut health changes occur as oestrogen and progesterone levels decline? Has this happened to you? And if you are experiencing insomnia, then your gut health (and liver health) suffers too – we forget that our digestive system operates on a 24 hour circadian rhythm as well.
The state of our gut health as well as the billions of microbes that make up our gut microbiome, is an important consideration in managing our menopause symptoms and/or our weight. That’s why I like some new research which has a spotlight on our changing gut health at this time of our lives (Peters et al, 2022).
It helps us to understand why we suddenly have some ‘urgency’ or IBS or constipation or the fact that bloating may have become worse during and after menopause. If your stomach feels distended, then you will know what I mean by this.
With so much going on in the lives of women in their peri-menopause to post-menopause years, increased stress and workloads, also contribute to insomnia. The result of all this, as well as the changes to our microbiome and the fact that our gut motility (movement) changes, means that bloating and discomfort can be a daily distraction.
That’s why in this post I have some gentle reminders for you and my 4 Factors to Forget Bloating are below if you scroll down.
If you are feeling bloated then one of the first things you can do to help release and reduce your bloating and gas is some gentle stretches such as in the image below. This type of stretch is known to gently massage the abdominal organs and gallbladder, thus releasing tension.
Yoga Instructors call it Pavanamuktasana (pah-van-ah-mook-TAHS-uh-nuh) — or the Wind-Relieving Pose. These types of stretches also help your lymphatic system which changes as we age. Helping our gut and colon to move trapped air and gas through gentle movement and stretching is important.
As we move through menopause, our changing oestrogen levels impact the tiny microvilli that line our digestive system, causing ‘gaps’ to increase between them. This is known as leaky gut syndrome. It can lead to IBS.
That’s why stretching is important.
When we stretch and do specific exercises, these help to move bile from our gallbladder into our gut, thus helping waste products to move along the intestines. Menopause hormonal changes impact a lower production of bile and storage, hence this can be part of the reason for feeling bloated as menopause arrives.
I didn’t fully understand the various changes to our organs as we move through menopause – did you?
Numerous women are relying on supplements to help them feel better, but as I discovered, this may only be a band-aid as they stop working into the longer term when women don’t adapt and adjust their lifestyle.
However, to ease bloating and increased gas, both of which are signs of Leaky Gut Syndrome, which for many of us, arrives during peri-menopause, then we need to make a few lifestyle changes too.
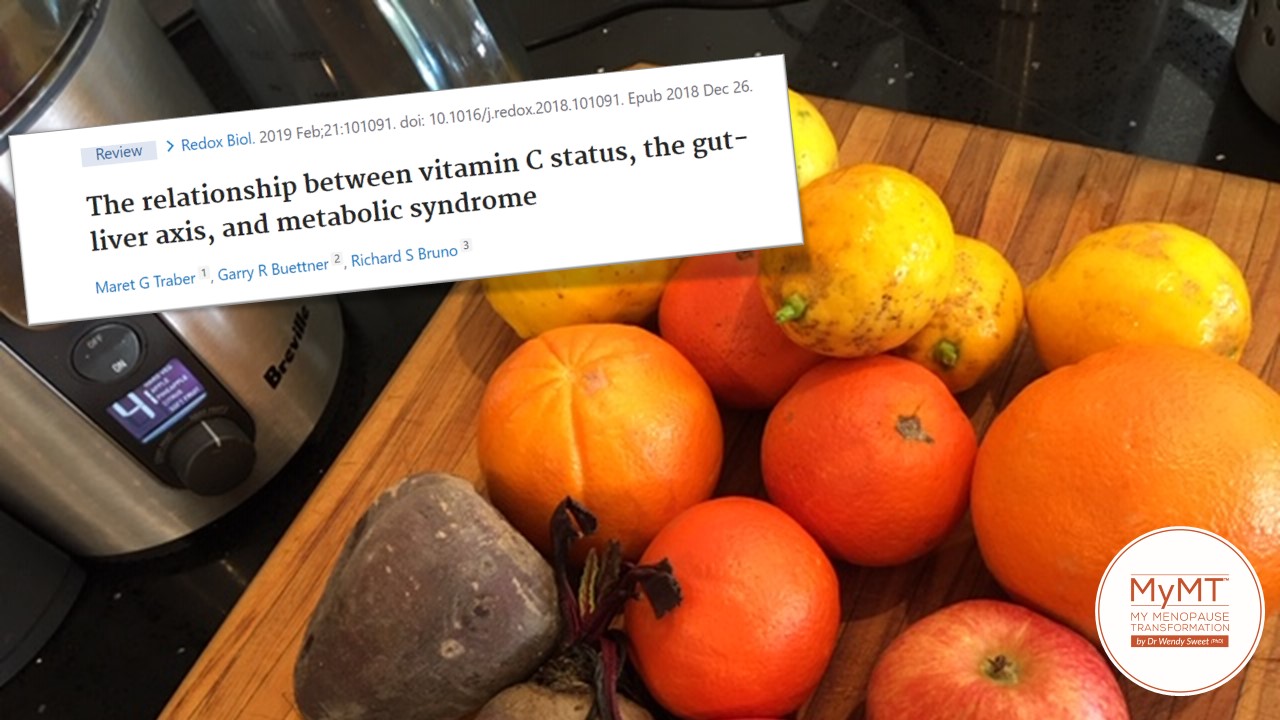
For example, gut health research suggests that our Vitamin C status has a greater influence that we think on the gut-liver axis and this in turn, influences metabolic syndrome (Traber et al, 2019), which is the condition that can lead to weight gain and cardiovascular problems as well as Type 2 diabetes.
With so many women experiencing changing gut health as they move into their 50s, I hope you like my article this week. And rest assured, if your gut health has changed, then you aren’t alone.
In western countries Irritable Bowel Syndrome [IBS] is 4 times more common in women as they reach mid-life.
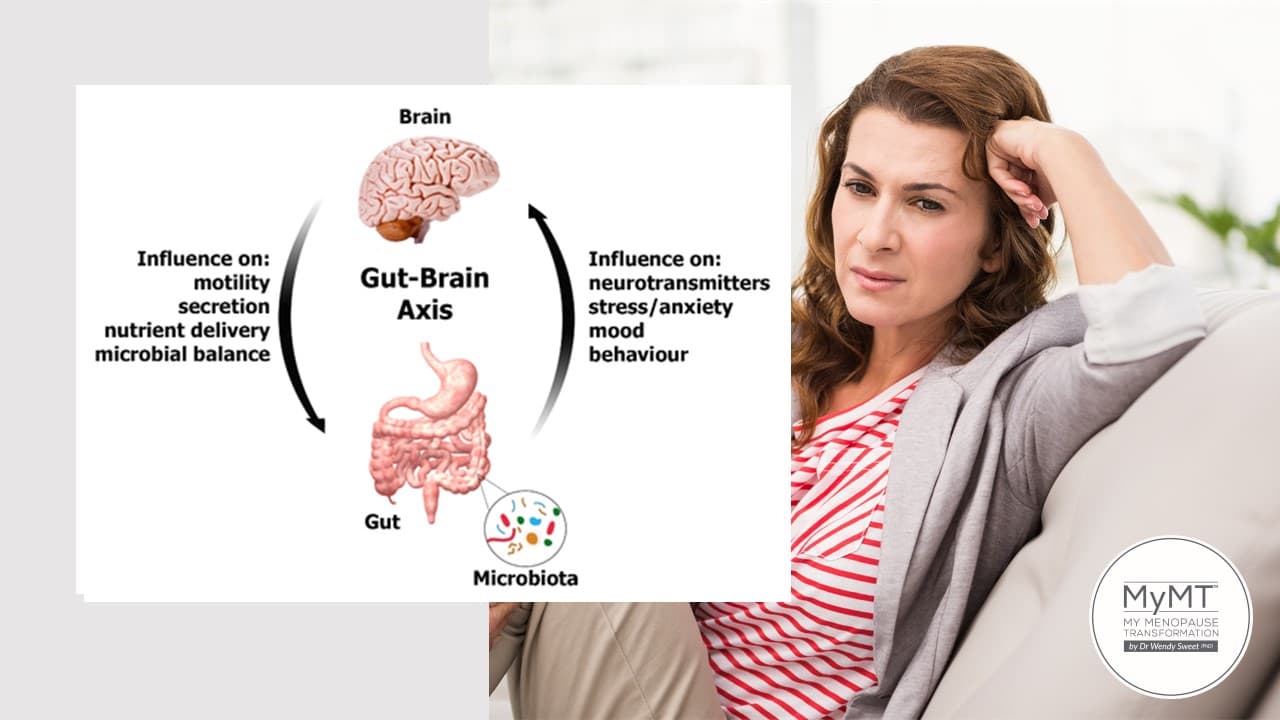
IBS impacts numerous menopause symptoms – depression, anxiety, weight gain (or loss) and brain-fog, sore joints, hot flushes and of course, menopause insomnia. All these symptoms are affected by changing gut health.
One of the main effects oestrogen has in our body, is to support our digestive health. In our monthly cycle, oestrogen was cycling up and down, and this meant that the higher levels of oestrogen helped our gut enzymes to work more efficiently.
The role of enzymes in your body is important. They work hard every second of every day to produce chemical reactions in the body.
For example, there are enzymes that help our digestive processes. When you eat that bit of bread, amylase is the enzyme that breaks down the starch in it. Amylase is present in your saliva. Then there is another enzyme called pancreatase. This is produced by our pancreas to help break down fats and proteins.
But here’s the thing – when we move from peri-menopause into menopause, the time of our life when our oestrogen levels decline, the production of these enzymes is reduced. Only since 2015, have researchers begun to understand that oestrogen has a role in helping the gut epithelium or lining to turn over cells regularly.
According to Dr Marek Glezerman, author of ‘Gender Medicine’ which explores the gender differences in health and disease,
“Functional Disorders of the digestive tract, such as Irritable Bowel Syndrome (IBS) is four times more common in women living in Western countries during and after menopause. In Japan, China, India and other parts of Asia, the ratio is the opposite.”
I love research that peaks my curiosity. I too developed gut and digestion problems as I moved through menopause, as have numerous women on my 12 week MyMT™ programmes too. Which is interesting, because I always look to see if they are on anti-depressant medications at the same time. If they are, then I ensure that they understand that current research now allows us to understand the connection between menopause depression and our gut health.
Therefore, if women are intent on getting off anti-depressants with their Doctor’s support, then they must also work towards restoring their gut health.
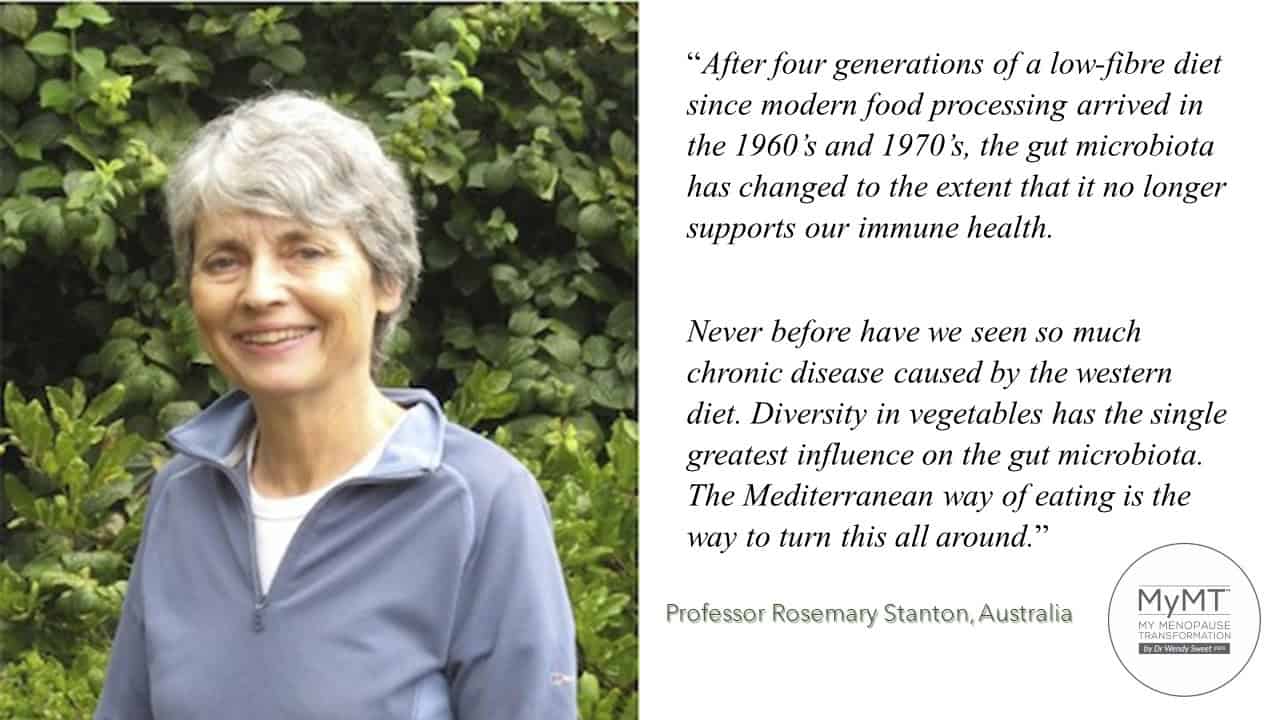
There’s also something else impacting on our gut health though and I have Australia’s Professor Rosemary Stanton to thank for my light bulb moment with understanding this. When I heard Professor Stanton speak at this year’s Lifestyle Medicine conference in Australia, my ears pricked up:
“After four generations of a low-fibre diet since modern food processing arrived in the 1960’s and 1970’s, the gut microbiota has changed to the extent that it no longer supports our immune health. Never before have we seen so much chronic disease caused by the western diet. Diversity in vegetables has the single greatest influence on the gut microbiota. The Mediterranean way of eating is the way to turn this all around.”
Not only are we are the first generation to come into menopause having experienced so many changes to our food environment, but we are also the first generation to have been exposed to substances that have a negative effect on our gut bacteria. And according to researchers, one of the greatest influences on our gut health has been our exposure to antibiotics.
The gut microbiome is one of the largest organs in the body (along with our skin) and we need to factor it into our menopause symptom management, especially if your energy is low. Gut health researcher, Professor Thomas Borody from Australia, reports that the gut is responsible for producing 70% of our energy.
There is also a powerful connection between your gut and your brain (which is why our gut is now referred to as our ‘second brain’), therefore many symptoms that we experience in menopause, such as foggy brain, depression, anxiety, insomnia and mood swings are now also being linked to the health of your gut micro-biome.
Imagine what happens to your energy levels, sleep, health and moods, when your gut isn’t performing to its best? It’s Ok, don’t answer that – I already know.
Gut health management is becoming an essential part of health restoration strategies and this is why, I now have an optional webinar on our changing gut health in menopause and post-menopause in my programmes. As Sylvia from the UK discovered, it’s an important consideration in managing menopause weight gain.

Knowledge of the gut-brain connection has increased 10-fold over the past decade. This has been due to improved brain research as well as genetic research into the gut microbiome. Both have opened the door to better understanding gut health and the link to disease, especially the effect of the accumulation of inflammatory changes as we get older.
With menopause heralding in the transition towards our ageing, this is a critical time of life to sleep all night, restore health to our body and for those of you who need to lose weight, this will also have a positive impact on your gut health, anxiety levels and daily energy too.
4 Factors to Help Manage your GUT HEALTH:
Once we understand the powerful connection between the brain, the gut, the vagus nerve, existing gut inflammation AND menopause, then we need to focus on these three factors:
Sleep All Night – as I keep saying to women, if you aren’t sleeping, then you aren’t healing and your heart rate stays higher during the day. This alone makes you feel more anxious because your nervous system stays ‘wired’ all day long and in turn this stimulates your gut which is serviced by the same nerves as your heart. As I’ve often mentioned before, our gut is also on a 24 hour circadian rhythm as are all of our major organs, so we need to improve our sleep in order to improve our gut.
Allow your gut to empty fully and heal overnight –
I encourage women as much as possible to allow their digestive system to rest for 12 hours overnight. This means that the timing of food and fluid is important. If we can avoid food for around 12 hours overnight (this changes obviously for shift-workers) then our digestive system gets the chance to actually digest and absorb the food that we eat during the day.

- Improve Your Food Quality and Vegetable Diversity – Professor Rosemary Stanton of Australia has been studying the health of the population in Australia for over four decades now: “The way to heal the gut is to have diversity in vegetable intake and increase fibre. This is what the gut has been designed for. Decades of low fibre, processed foods have resulted in worsening health of the population and a plethora of diseases which are mainly related to our changing food environment.”

- Move and Stretch More – try to move in ways that help your lymphatic system, gallbladder and colon to release tension. This includes the yoga poses that I shared with you earlier as well as swimming, rebounding and performing exercises that improve your breathing. I have all of these workouts in the MyMT™ Rebuild My Fitness programme for you. I hope you can join me on this fabulous 12 week exercise programme if you are wanting to stay healthy through exercise.

I hope you can join me sometime.

References:
Glezerman, M. (2016). Gender Medicine. Duckworth & Co Publ.
Nie, X., Xie, R. & Tuo, B. (2018). Effects of Estrogen on the Gastrointestinal Tract. Dig Dis Sci 63, 583–596
Peters BA, Santoro N, Kaplan RC, Qi Q. Spotlight on the Gut Microbiome in Menopause: Current Insights. Int J Womens Health. 2022 Aug 10;14:1059-1072.
Qin R, Tian G, Liu J, Cao L. The gut microbiota and endometriosis: From pathogenesis to diagnosis and treatment. Front Cell Infect Microbiol. 2022 Nov 24;12:1069557.
Traber MG, Buettner GR, Bruno RS. (2019). The relationship between vitamin C status, the gut-liver axis, and metabolic syndrome. Redox Biol. 21:101091. doi: 10.1016/j.redox.2018.101091.
Veira, A., Castelo, P. et al, (2017). Influence of oral and gut microbiota in the health of menopausal women. Front. Microbiol. 8, 1884. https://doi.org/10.3389/fmicb.2017.01884



