Every week I think to myself, ‘what might you like to read about when it comes to better understanding your menopause transition’? In pondering this, I often seek inspiration from women on my programmes or from some of you who have emailed me with your questions as you come into the MyMT™ community via my symptoms quiz, my newsletter or via facebook.
This week, the answer to my question was easy. Women discussing their weight loss and symptom management strategies in my private coaching group. With a few of them in post-menopause and struggling to sleep because of night sweats, I’ve been telling them to get their iron and ferritin levels checked.
Many women on my programme are still quite active. But few understand that as we move through menopause, there are changes to our iron and ferritin (stored iron) levels. Iron plays an important role, not only in oxygen delivery to the tissues, but also as a cofactor with several enzymes involved in energy metabolism and regulation o four body temperature.
Over the past 8 years since setting up MyMT™, I’ve received emails from women living in different countries, who are on my programmes who have sent me some of their blood results to look at.
I don’t normally do this (and I never interfere in medical decisions as I am not a medical Dr), but if they aren’t resolving their sleep or overnight hot flushes, I like to check what their blood work might say about their iron or stored iron (ferritin) levels. Esepcially if they are exercising or have active jobs or are competing in Masters Sports, or conversely, they are sedentary and overweight.
As a sports and exercise physiologist, I taught for decades that when female athletes are low in iron, then they feel chronically tired, hotter than normal (or cold) and don’t sleep well due to night sweats. This is known as athlete anaemia.
However, for women who aren’t athletes or are menstruating, conversely, we have to think about high iron levels or iron overload. This condition differs from haemachromatosis, which is a medical condition that requires a medical diagnosis and monitoring, so for those of you in post-menopause, this is a reminder to get your bloods checked sometime.
If your iron or ferritin levels are too high, (or conversely, too low, then your hot flushes and night sweats and weight gain may stay around, despite all the supplements you may be taking. High iron levels are also associated with post-menopause heart disease, so it’s worth checking out.
It’s an important topic for all women in menopause yet, seems to be being forgotten about in all the discussions that I hear. So, here it is, a great topic for you to know about as you transition menopause – your changing iron levels as you age.

Iron is a mineral that I talk a lot about in the MyMT™ programmes.
Whilst many of us are aware of how important this mineral is in pregnancy and lactation as well as when we are growing up, we often forget how important it is to manage during our menopause transition. Recently, new research suggested that blood iron levels could play a role in influencing how long you live.
Having too much or too little iron in the blood (iron overload or iron depletion) appeared to be linked to an increased risk of cardiovascular disease, stated the lead researcher, Paul Timmers from the University of Edinburgh. ‘Study of Over 1 Million People Finds Intriguing Link Between Iron Levels And Lifespan’ said the headline. Knowing that iron is important to balance as we move into post-menopause, this got my attention.
“We are very excited by these findings as they strongly suggest that high levels of iron in the blood reduces our healthy years of life, and keeping these levels in check could prevent age-related damage. We speculate that our findings on iron metabolism might also start to explain why very high levels of iron-rich red meat in the diet has been linked to age-related conditions such as heart disease.” (Lead Researcher, Dr Paul Timmers, Univ. of Edinburgh)
For women in post-menopause, this is important news and suggests that yes indeed, we do need to change our diet as we get older as I promote in the MyMT™ programmes.
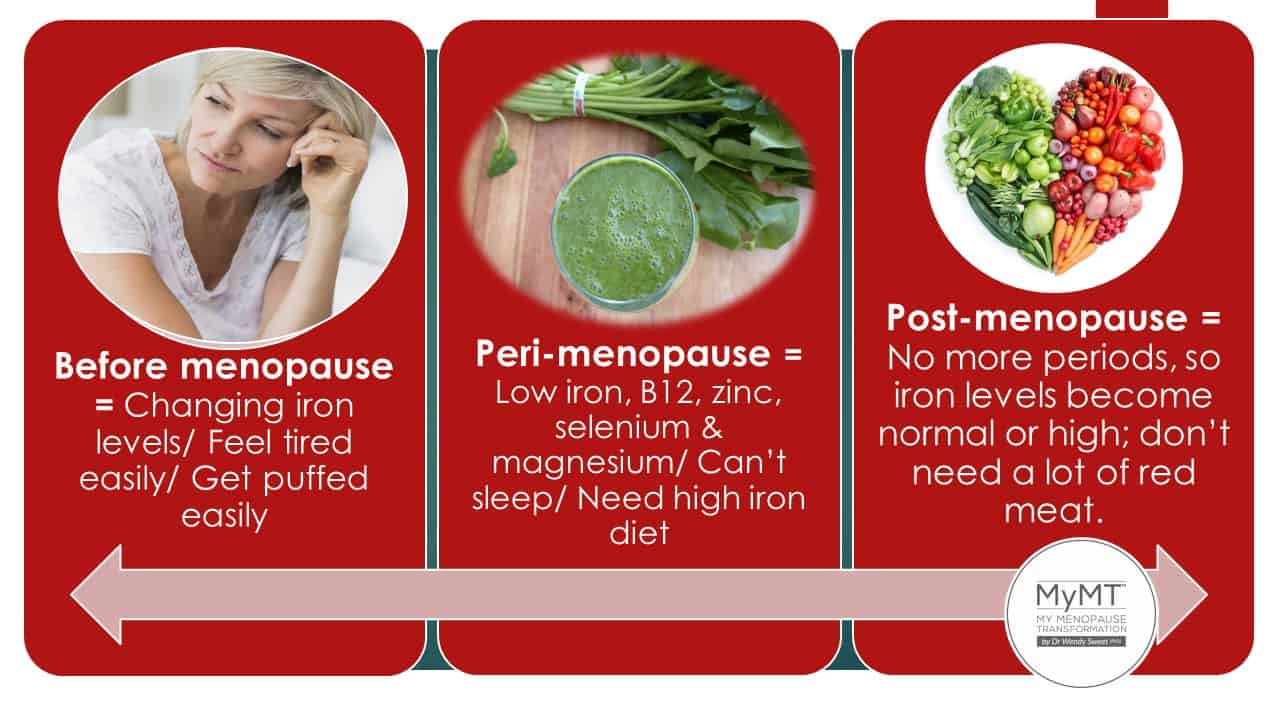
But it’s not just about those of you in post-menopause either. If you are in peri-menopause (mid to late 40’s) and still menstruating, then you need to manage your iron levels too. Your needs are greater than those of us, who aren’t menstruating any more.
If your iron stores (ferritin) are too low, then you may have developed iron-deficiency anaemia. If this is the case, then your sleep will be disturbed and your heart rate may be higher overnight, causing increased anxiety, palpitations and hot flushes.
And yes, you will feel exhausted as well. If you are a runner or exerciser and feeling tired all the time and your hot flushes have increased, then do please check your iron and stored iron levels, especially if you are transitioning through menopause. Let me explain why.
If your red blood cells are low in iron, then you don’t have enough oxygen molecules attaching to them. That’s what iron does.
It is a crucial player in your oxygen transport system. If your iron levels are low, then your heart has to work harder to pump oxygenated blood to your vital organs.
This higher workload of your heart may be especially apparent overnight, because this is when your body is trying to rest and restore your immune system.
If your heart has to work harder to deliver oxygentated blood to your cells, then your heart rate increases as does the work of your thyroid. Hence, you overheat. If you are suffering from night sweats and you are constantly fatigued and you are in peri-menopause, then please check your iron and ferritin levels.
However, if you have stopped menstruating, and you are experiencing symptoms that may include joint pain, muscle weakness, fatigue and increasing hot flushes, then you could be experiencing iron overload, especially if you eat a lot of high iron foods and meat. [NB: This differs from the genetic condition called hemachromatosis which some women also have]. We often don’t think about our iron needs in post-menopause, but we need to – because when you aren’t menstruating any more, then your iron needs change.
Iron Levels and Menopause: Does Increased Iron Affect the Health of Postmenopausal Women?
Iron and ferritin balance as we move through menopause is something that I’ve been talking about in the MyMT™ programmes for a few years now.
I’ve been intrigued by post-menopause women still getting hot flushes and night sweats and with the cessation of menstruation, I’ve always wondered whether an increase in iron levels in post-menopause could increase hot flushes and cardiovascular risk as women age. It seems the answer might be yes.
By examining ferritin data from the NHANES III study, researchers found that serum ferritin levels are parallel with the reported prevalence of hot flashes among African-American, white, and Hispanic women. This observation suggests that, in contrast to iron deficiency leading to cold intolerance, an increase in iron might play a role in post-menopausal hot flushes.
This makes so much sense to me. You see, as we move into post-menopause, we aren’t menstruating any more. Oestrogen and iron are two of the most important growth nutrients in a woman’s body development. Oestrogen affects the growth, differentiation, and function of tissues such as breasts, skin, and bone.
Iron is essential for oxygen transport, DNA synthesis, as well as energy production.
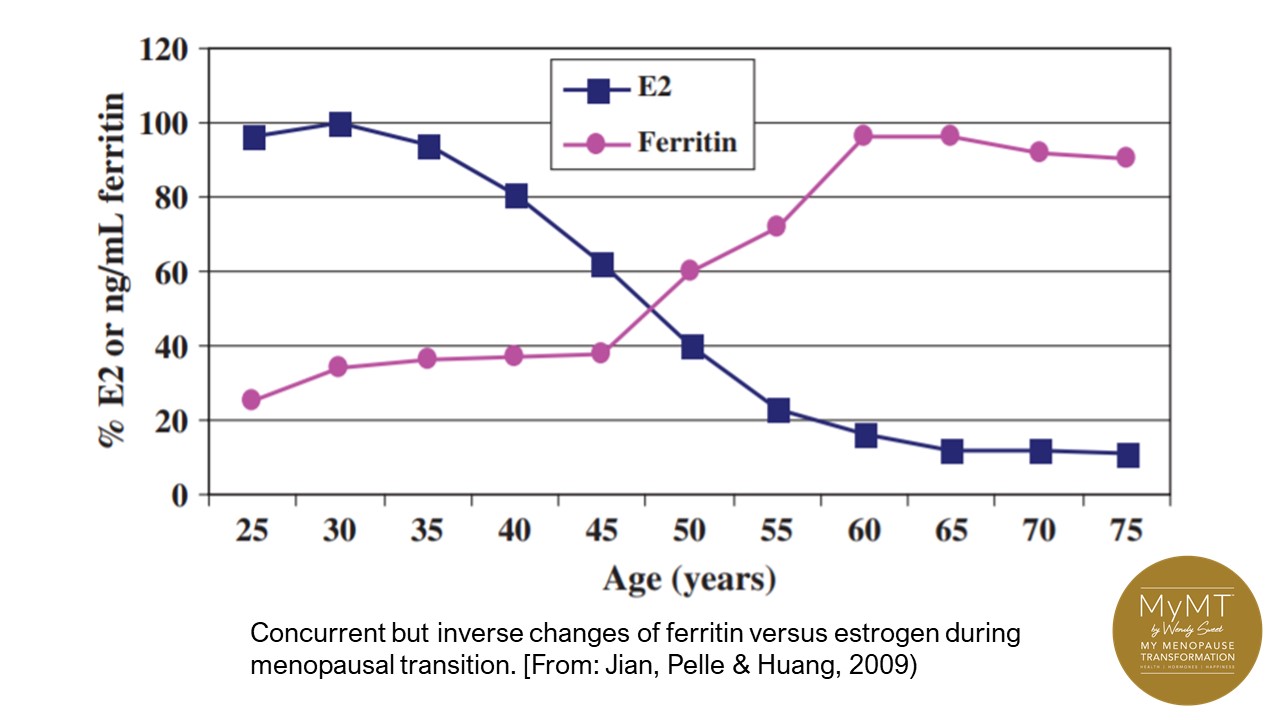
With the iron data obtained from the Third National Health and Nutrition Examination Survey (NHANES III), results showed that concurrent but inverse changes occur between iron and oestrogen levels in healthy women during their menopausal transition.
Whereas oestrogen decreases because of the cessation of ovarian functions, iron increases as a result of decreasing menstrual periods. For example, the level of serum ferritin is increased by two- to threefold during this transition into cessation of menstruation. High serum ferritin stresses the cardiovascular system and temperature regulation mechanisms.
How much Iron is enough?
Important differences exist between men and menopausal women in terms of timing and patterns of changes in hormone and iron levels. First, iron increase in men happens in conjunction with the increase of male reproductive hormones, which could provide protection against the harmful effects of the increased iron.
Nevertheless, iron increase in women occurs during their midlife (age 42–51 years) at the same time as female sex hormones are decreased as you can see from the image below.
In my 12 week online MyMT™ programmes I talk about our changing iron needs as we age.
If you are in peri-menopause (and an exerciser) then look at around 12 mg a day. If you are in post-menopause, then bring this down to around 8-10mg a day. And yes, get your blood levels checked with your Doctor as you move through menopause and if all those supplements you are taking for menopause hot flushes aren’t working as you move into post-menopause, then please don’t waste your money. Get your iron and ferritin levels checked instead.
Your iron balance during your menopause transition is greatly influenced by two main factors:
- The composition of your diet.
- The health of your liver and small intestine – both important sites of iron metabolism and absorption.
Two broad categories of iron are found in your food. The first category is called haem iron. This is more readily absorbed iron and comes from red meat and fish sources.
The second category is non-haem iron. This is sourced from various plants, legumes and grains. Sources of non-haem iron can be problematic however, because this form of iron is influenced by other constituents of your diet. Some are ‘promoters’ and some are ’inhibitors’.
For example, the most important ‘promoters’ of non-haem iron are foods high in Vitamin C and/or meat. For vegans and vegetarians who are in peri-menopause, this is important to understand. Add Vitamin C to your plant-based meals.
Iron absorption is also under the influence of ‘inhibitors’, i.e. constituents of foods that prevent enough iron being absorbed through the gut wall. Known ‘inhibitors of iron’ include phytates in some plants and tannins in tea, coffee and wine.
And please don’t forget that with the gut wall being the site of iron absorption, then your gut health is important for iron absorption too (if you have gut health issues or IBS then please look at my brand new Gut Health module) or come on board into the 12 week programme as my bonus modules are all part of the extended programmes as well.
Women going through menopause and into post-menopause, who aren’t sleeping and experiencing emotional changes, sore joints, weight gain and more, are doing it tough – even more so, considering the challenges over the past couple of years.
That’s why I would love you to know the information that I have for you in the programmes that I’ve designed from my women’s healthy ageing research. I would love to support you and my mid-year JULY weight loss sale for women in post-menopause has now opened.
There are also Success Stories and Testimonials that amazing women have kindly shared too. Please do spend some time exploring their stories if you aren’t sure about coming on board with me.
If you’ve got time for some additional reading there are numerous BLOGS on my website to distract you from the chaos of the world too. It’s such a privilege to have you with me in the MyMT™ community and remember that while I live in New Zealand at the bottom of the world, I’m only an email away if you have any questions about the programmes – wendy@mymenopausetransformation.com
Wendy Sweet (PhD)/ Member: Australasian Society of Lifestyle Medicine.
Related Tag: Menopause AU
References:
Bozzini, C., Girelli, D. et al, (2005). Prevalence of Body Iron Excess in the Metabolic Syndrome. Diabetes Care, 28 (8): 2061–2063. https://doi.org/10.2337/diacare.28.8.2061
Franchini, M., Targher, G., Montagnana, M., & Lippi, G. (2008). Iron and thrombosis. Annals of hematology, 87(3), 167–173. https://doi.org/10.1007/s00277-007-0416-1
Herber-Gast G, Brown WJ, Mishra GD. (2015). Hot flushes and night sweats are associated with coronary heart disease risk in midlife: a longitudinal study. BJOG. 122(11):1560-7. doi: 10.1111/1471-0528.13163. Epub 2014 Nov 7. PMID: 25377022.
Jinlong Jian, Pelle, E. & Xi, H. (2009). Iron and menopause: Does increased Iron affect the health of postmenopausal women? Antioxiants & Redox Signaling Journal, 1(12), 1-6.
Murday HK, Rusli FD, Blandy C, Vollenhoven B. (2016). Night sweats: it may be hemochromatosis. Climacteric. 19(4):406-8. doi: 10.1080/13697137.2016.1191461. Epub 2016 Jun 14. PMID: 27296845.
Timmers, P.R.H.J., Wilson, J.F., Joshi, P.K. et al. (2020) Multivariate genomic scan implicates novel loci and haem metabolism in human ageing. Nat Commun 11, 3570. https://doi.org/10.1038/s41467-020-17312-3


