Knowledge about how the gut-microbiome alters aspects of our immune, metabolic and nervous system health has increased 10-fold over the past decade.
Fortunately, some of this knowledge has also been situated in midlife women’s health.
Whilst this increase in research has been mainly due to improved genetic research, it’s also arrived from advances in microbial technology. Both have opened the door to better understanding of gut health and the link to inflammatory diseases as women age.
In western countries Irritable Bowel Syndrome [IBS] is 4 times more common in women as they reach mid-life – also a time of life, when menopause symptoms may cause so much frustration.
With my own gut health changing when I reached my early 50s, it made sense to me that these issues may well be related.
As it turns out they are, and with the huge number of women on my 12 week lifestyle programmes mentioning that they feel that their gut health has changed since arriving in menopause, I wanted to explain why.
One of the main effects of oestrogen is to support digestive health.
In the usual monthly menstrual cycle, oestrogen cycles up and down. Oestrogen levels rise during the mid-follicular phase and then drop precipitously after ovulation. This is followed by a secondary rise in oestrogen levels during the mid-luteal phase with a decrease at the end of the menstrual cycle. [Reed & Carr, 2018].
During the higher oestrogen phases, gut enzymes work more efficiently.
Understanding the role of gut enzymes and their connection to oestrogen levels is important.
They work hard every second of every day to produce chemical reactions in the body. For example, there are enzymes that help our digestive processes.
When you eat that bit of bread, amylase is the enzyme that breaks down the starch in it. Amylase is present in your saliva. Then there is another enzyme called pancreatase. This is produced by our pancreas to help break down fats and proteins.
But here’s the thing; when we move from peri-menopause into menopause, when our oestrogen levels decline, the production of these enzymes is reduced.
Menopause HRT doesn’t change this which is why many of your clients may find that their HRT isn’t helping their gut health and microbiome changes.

Only since 2015, have researchers begun to understand that oestrogen has a role in helping the gut epithelium or lining to turn over cells regularly. According to Dr Marek Glezerman, author of ‘Gender Medicine’ which explores the gender differences in health and disease,
“Functional Disorders of the digestive tract, such as Irritable Bowel Syndrome (IBS) is four times more common in women living in Western countries during and after menopause. In Japan, China, India and other parts of Asia, the ratio is the opposite.”
The nature of menopausal symptoms is common to all women, however, geographical location and ethnicity influence the prevalence of certain symptoms. (Hunter, Chedraui et al., 2012).
This bought my attention to the possible link between changing gut health in midlife women and the frequency of severity of hot flushes, weight gain and other symptoms.
Another important realisation about changes to gut health with age, is the link between certain types of microbes that reside in the colon and how these impact health problems as women age.
For example, in women with menopause-related osteoporosis, scientists have discovered that the microbial organism called Prevotella may be protective against this life-changing bone disease.
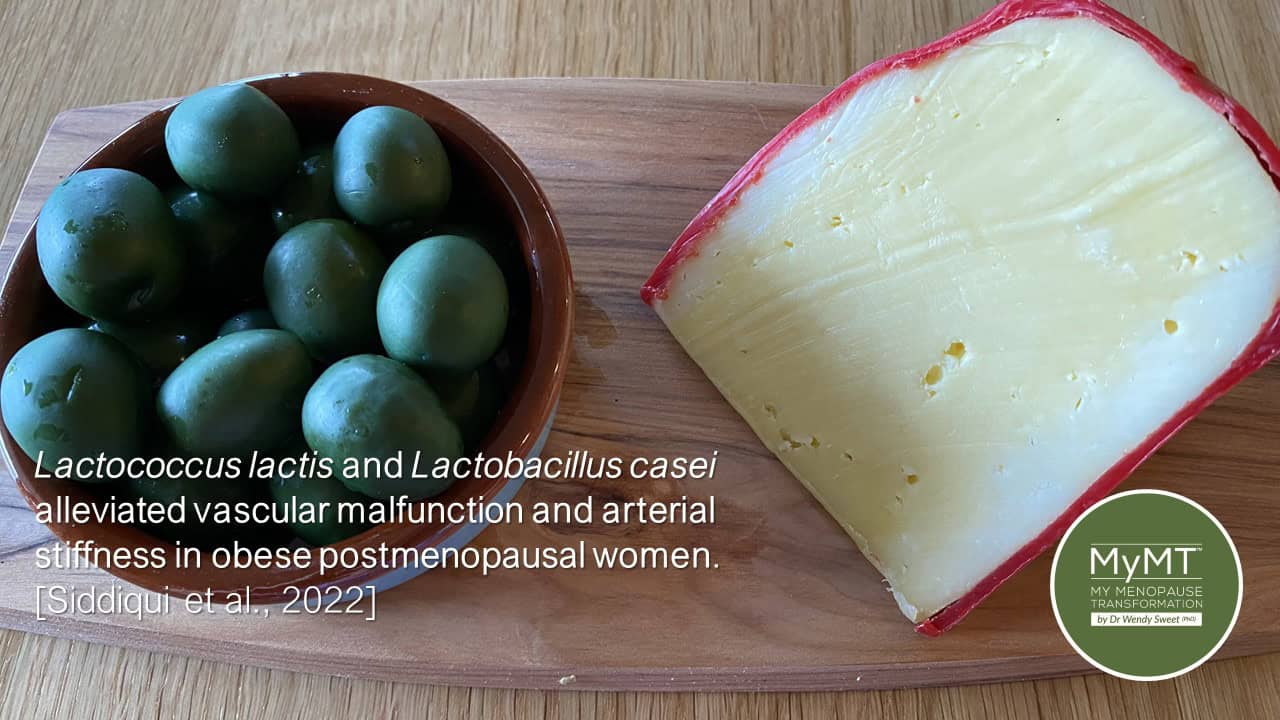
And when it comes to women’s heart disease, it seems that optimal numbers of Lactobacillus Casei may help to reduce vascular stiffness.
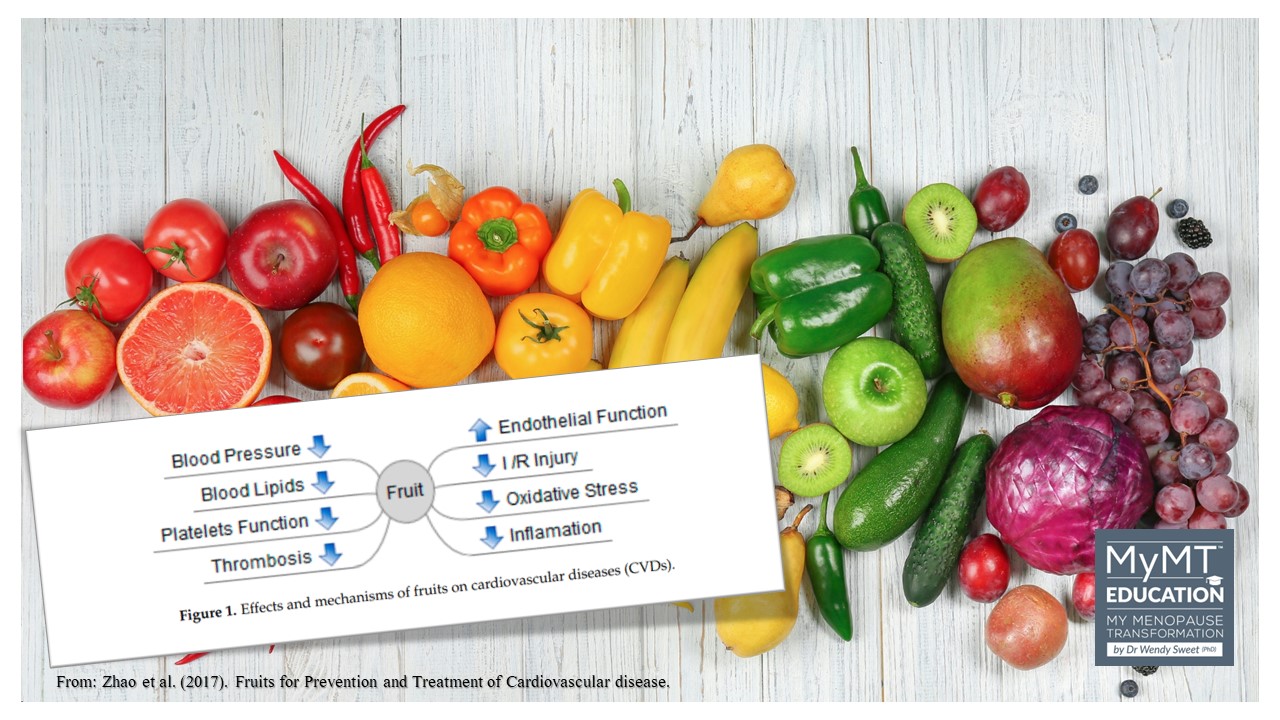
As those of you who have undertaken my Practitioner course know, this condition is associated with women’s ageing blood vessels during and after menopause, which can contribute to high blood pressure (hypertension). [Siddiqui et al, 2022]. It’s also why your female clients need to increase their intake of fruits to help prevent cardiovascular disease.
Unnatural shifts in the gut microbiota composition, known as dysbiosis, can lead to several health disorders. Knowing that one of these disorders is to do with temperature regulation problems, is important for women transitioning into and through menopause.
That’s why, whether your clients are on menopause HRT or not, looking after gut health is an important lifestyle strategy for you to promote as part of your coaching with midlife and older women.
Numerous factors impact our gut function over our lifetime. This includes our diet, environmental changes (extreme heat and cold), antibiotic exposure, sleep disturbance, physical activity (too much or not enough), hormonal changes and pathological or disease stimuli – all of these factors cause a shift in the gut microbiota. Hormonal changes during menopause are included in this list too.
‘One of the factors that plays a pivotal role in microbiota modulation, although broadly understudied in current research, is the change in female sexual hormones throughout life, including menopause.’ [Veira, A., Castelo, P. et al, (2017)]
The role of oestrogen in our gut health is more important than we think. Throughout our life, and more so after puberty, oestrogen helps to keep inflammation in our intestines at bay. It does this by preventing us from developing what is known as ”leaky gut’.
Researchers have discovered that dysregulation of oestrogen receptors in the intestinal mucosa of patients with Crohn’s Disease and Ulcerative Colitis indicates that oestrogen signaling plays a role in the local immune response in the intestine, helping to maintain the integrity of the gut lining, called the epithelium.
The interesting thing is that this is known to occur in a gender- and age-dependent manner (Jacenik, et al. 2019). So, for women transitioning through menopause, from their mid-40s on, the decline in oestrogen levels impacts our gut health. This may result in a leaky gut and dysbiosis from a changing microbiome.
In turn, the subsequent inflammatory changes in our bowel can increase the frequency and severity of hot flushes. When inflammatory changes are present in the body, your body’s natural defence mechanisms are to try to cool you down. Hence, as you already know from when you were sick or had a fever, you begin to sweat.
Hot flushes and night sweats are a sign that your body is trying to cool down.
It’s no surprise to me that many menopause supplements have ingredients that are known to improve the gut microbiota … but my challenge to you is what are you doing about your diet and sleep? These factors impact your gut health too.
What all this means is that if your clients want to reduce their symptoms during menopause and manage their weight, then sorting out gut health matters.
This is why I have a module about restoring Gut Health as part of my restoration series and you or your clients can purchase this as a stand-alone module.

3 Strategies to Teach Your Midlife Clients:
The gut microbiome is one of the largest organs in the body (along with our skin) but here’s what blew me away with the research. Gut health researcher, Professor Thomas Borody from Australia, reports that the gut is responsible for producing 70% of our energy.
There is also a powerful connection between the gut and the brain (which is why our gut is now referred to as our ‘second brain’).
Therefore many symptoms that women experience in menopause, such as foggy brain, depression, anxiety and mood swings can also be linked to the health of their gut micro-biome. I might also add insomnia in there too.
If this sounds familiar to you with the clients you are working with, then here are 3 strategies to get you started on helping your clients:
- Menopause hormonal changes cause gut motility (called peristalsis) to slow down. Understanding this means that women should slow down the amount and frequency of their food intake. Portion control is important as is their overnight fasting for 12-14 hours. This allows time for the food already in the gut to be digested and absorbed.

2. Clients should maintain optimal temperature regulation – not extreme heat or cold. This is difficult with climate change in many countries I know. However, environmental temperature and heat stress are known to modify the gut microbiome. Changes in core temperature have been linked to altered microbiome composition and function.
Those of you living in regions such as the Northern parts of Australia, need to keep this in mind, with your clients. Extreme summer heat causes worsening gut health. (Hylander & Repasky, 2019).
The opposite is true for those women living in countries that have extremes in cold, such as in Northern Canada. As such, reducing exercise intensity in extreme heat or cold environments is recommended.
3. Changing the diet is important as is restricting fats and increasing Vitamin C intake. New research reports that high fat diets mimic the effects of a western diet (Lobionda, Sittipo et al, 2019) and this increases bowel inflammation. Hence, the type of fat your clients have matters, as do the foods that supply your gut microbiota with good bacteria. Prebiotic foods are rich in dietary fibres.
So, what you’re clients need are fruits, vegetables, wholegrains, and pulses. The gut can’t digest these fibres, so they travel to the gut where they feed the good bacteria that make butyrate.
This is a primary nutrient that is physiologically produced by the microbial fermentation of dietary fibres. It plays a functional role in maintaining the integrity and function of the intestinal cells. (Leonel & Alvarez-Leite, 2015).
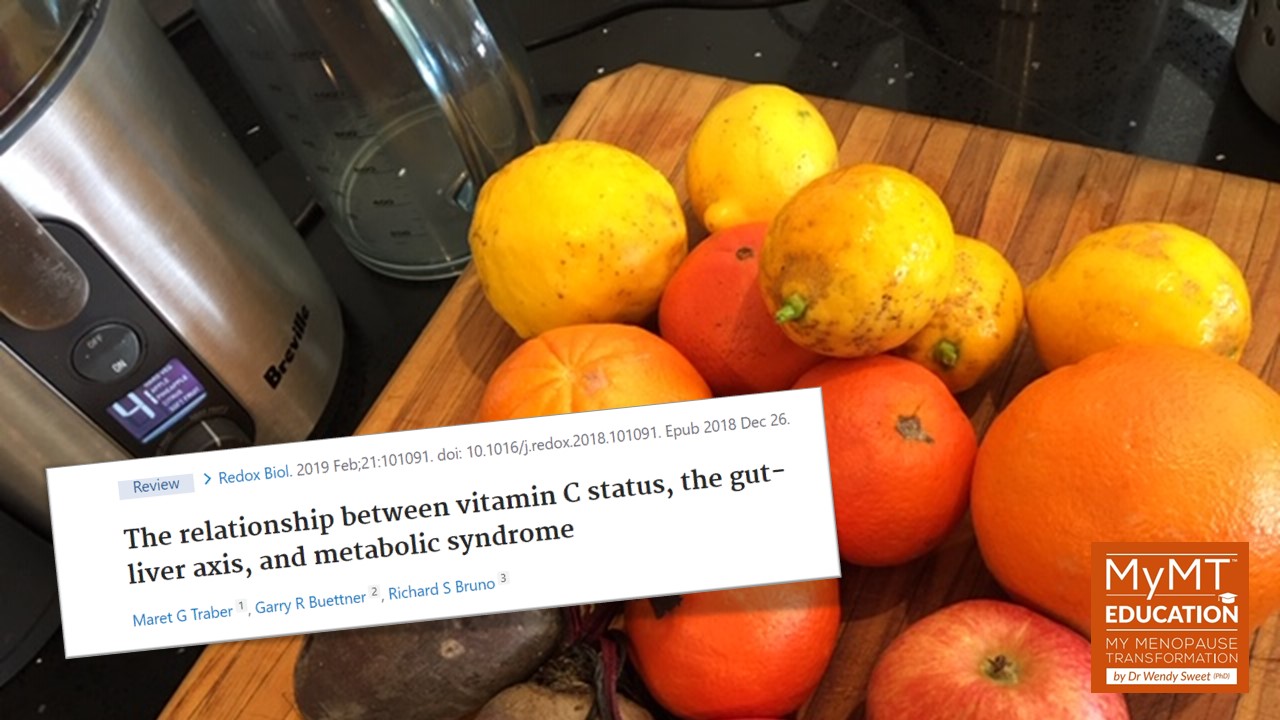
Furthermore, studies also indicate that Vitamin C is needed to help prevent Intestinal Bacterial Overgrowth (IBO), which is a complication of the increased visceral fat that can arrive during menopause. (Traber, Buettner et al, 2019).
New research is also emerging about the role of the gut microbiome in certain women’s health problems. Hence, promoting foods that increase certain healthy microbes in the gut and reduce harmful microbes is an interesting and emerging research purpose, so watch this space!
For example, new evidence on the connection between changing gut microbes and women’s health issues suggests that the microbes, Lactobaccillus casei and Lactococcus lactis help to alleviate vascular malfunction and arterial stiffness in overweight post-menopausal women [Siddiqui, Makhlouf et al., 2022].
Two foods that supply these bacteria, include Green Olives and hard Cheese.
One of the most frequent messages that I give women on my own programmes, is that menopause isn’t ‘just’ about hot flashes, brain fog or anxiety, despite these being the main symptoms dominating public menopause discussions these days.
With interest growing in the dynamic role of gut microbiome disturbances in human health and disease and how oestrogen has a role to play in this, there is increasing justification for my message!
Dr Wendy Sweet (PhD)/ My Menopause Transformation
Come join me on one of the important MyMT™ Education Courses!

References:
Agnoletti D, Piani F, Cicero AFG, Borghi C. The Gut Microbiota and Vascular Aging: A State-of-the-Art and Systematic Review of the Literature. J Clin Med. 2022 Jun 20;11(12):3557.
Glezerman, M. (2016). Gender Medicine. Duckworth & Co Publ.
Hunter, Myra & Chedraui, Peter & Blümel, JE & Tserotas, Konstantinos & Aguirre, W & Palacios, S & Sturdee, David. (2012). The International Menopause Study of Climate, Altitude, Temperature (IMS-CAT) and vasomotor symptoms. Climacteric : The Journal of the International Menopause Society. 16. 10.3109/13697137.2012.699563.
Hylander, B. & Repasky E. (2019) Temperature as a modulator of the gut microbiome: what are the implications and opportunities for thermal medicine?, International Journal of Hyperthermia, 36:sup1, 83-89, DOI: 10.1080/02656736.2019.1647356
Jacenik, D., Cygankiewicz, A. I., Mokrowiecka, A., Małecka-Panas, E., Fichna, J., & Krajewska, W. M. (2019). Sex- and Age-Related Estrogen Signaling Alteration in Inflammatory Bowel Diseases: Modulatory Role of Estrogen Receptors. International journal of molecular sciences, 20(13), 3175. https://doi.org/10.3390/ijms20133175
Leonel, A. & Alvarez-Leite, J. (2012). Butyrate: implications for intestinal function. Review, Lippincott, Williams and Wilkin, 15 (5), 1-6.
Madison A, Kiecolt-Glaser JK. Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr Opin Behav Sci. 2019 Aug;28:105-110.
Monteleone, P., Mascagni, G., Giannini, A. et al. Symptoms of menopause — global prevalence, physiology and implications. Nat Rev Endocrinol 14, 199–215 (2018). https://doi.org/10.1038/nrendo.2017.180
Nie, X., Xie, R. & Tuo, B. (2018). Effects of Estrogen on the Gastrointestinal Tract. Dig Dis Sci 63, 583–596.
Reed B. & Carr B. The Normal Menstrual Cycle and the Control of Ovulation. [Updated 2018 Aug 5]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet].
Siddiqui, R.; Makhlouf, Z.; Alharbi, A.M.; Alfahemi, H.; Khan, N.A. The Gut Microbiome and Female Health. Biology 2022, 11, 1683. https://doi.org/10.3390/biology11111683
Tomova A, Bukovsky I, Rembert E, Yonas W, Alwarith J, Barnard ND, Kahleova H. The Effects of Vegetarian and Vegan Diets on Gut Microbiota. Front Nutr. 2019 Apr 17;6:47. doi: 10.3389/fnut.2019.00047.
Traber M., Buettner G., Bruno R. (2019). The relationship between vitamin C status, the gut-liver axis, and metabolic syndrome. Redox Biol. 21:101091.
Veira, A., Castelo, P. et al, (2017). Influence of oral and gut microbiota in the health of menopausal women. Front. Microbiol. 8: 1884.