“Accepting what we can and cannot change is one of the most important aspects of understanding resilience. It’s learning to work with and grow what’s right in our lives while accepting, but not putting all our energy into, what’s not.”
[Matthew Johnstone]
How are you coping with your menopause transition? And how are you coping with everything else going on in your life? I know myself, that this time of life can be tough and it has been for the thousands of women who have joined me over the years, so if you are feeling a bit confused then you aren’t alone!
But as we start to make some lifestyle changes which help to build our resilience to this time of life, then rest assured that we can start to feel more in control.
Developing resilience involves maintaining flexibility and balance in your life as you deal with stressful situations and/or if your menopause symptoms are the cause of feeling stressed and over-whelmed.
We often don’t think of this time of our life as contributing to our stress. However, as research from the Swiss Peri-menopause Study (Suss, Willi et al, 2021) reports, peri-menopause and menopause changes can really challenge our emotional and physical resilience – but interestingly, not for all women.
That’s why I love this new research.
Around the world during 2021, we’ve seen some amazing acts of fortitude. People dealing with difficult events that change their lives. Those of you who are still doing it tough with your immune system also know what I mean as do those of you working in the frontline of health-care or who have lost loved ones over the past year.
How is your resilience to all of these changes? I’m not surprised if you’re feeling a bit exhausted and have little resilience left. It was the same for Clinical Psychologist, Dr Clare – supporting NHS employees over the past 2 years left her pretty exhausted and low on resilience. I was so pleased when she came onto my programme when she did as I’m sure her workload isn’t getting any easier with the rise in cases in the UK as well as staffing shortages in health-care.

Resilience is my theme word as women join me on the MyMT™ programmes. It’s a word that the American Psychological Association (APA) defines as “the process of adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress,” or “bouncing back” from difficult experiences.”
What I like is that the APA’s definition is one of being a process versus a stable personality trait (often termed resiliency). This suggests that we all have the capacity to build and demonstrate resilience, regardless of our socioeconomic backgrounds, personal experiences, or social environments.
Many of us already know that our peri-menopause and menopause transition arrives with significant challenges to our physical and emotional state. Due to reproductive hormonal changes, many women experience hot flushes, night sweats, or sleep disturbances, but it is also a critical phase for the onset of psychological disorders such as depression and anxiety (Soares 2017).
Besides this, changes and transitions in social relationships may occur during menopause, such as children leaving home, the birth of grandchildren, marital tensions, or long-term care dependency or death of parents and of course, workplace challenges and other changes occurring (Schmidt et al. 2004). It can be a tough time of our lives as I learnt myself and as many other women discover and research continues to support that menopause and stressful life events are not compatible partners!
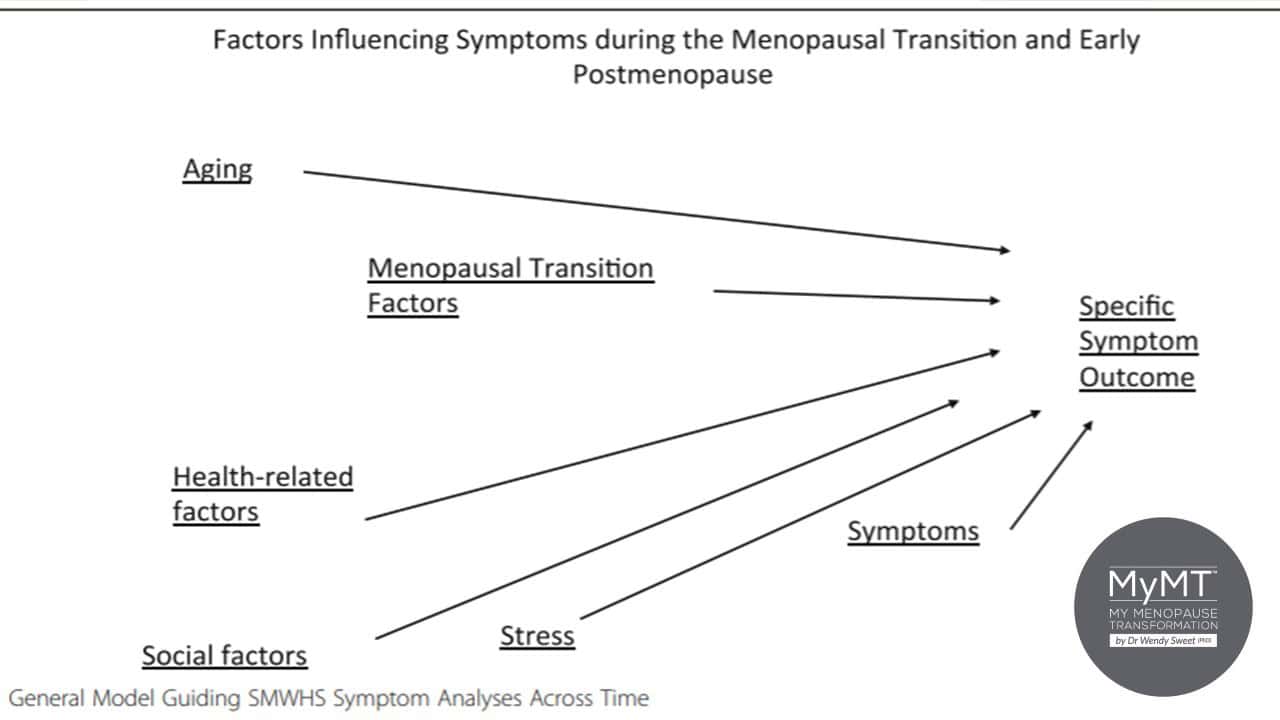
As physical and psychological transitions and challenges may have an impact on the psychological well-being of menopausal women, specific coping strategies are required for a successful adjustment (Ngai 2019).
Women who cope adequately with the challenges presented by menopause can be described as resilient (Brown et al. 2015).
Which is why I like this study out of Switzerland as part of the Swiss Perimenopause Study. It explored the resilience traits and behaviours of women who reported an overall positive well-being during menopause. They appeared to be resilient to the potentially negative effects of this life phase. (Suss, Willi et al, 2021).
These characteristics were:
- Optimism
- Emotional Stability
- Emotional Regulation
- Self-compassion
- Self-esteem.
These are all factors that are strongly related to women’s well-being as well as mental health in perimenopause.
Resilience is not a characteristic that people either have or don’t have. It involves behaviours, thoughts and actions that can be learned and developed by anyone.
And being resilient doesn’t mean that you don’t experience difficulty or distress. We all know that emotional changes are common in people who have had to cope with trauma or adversity in their lives, but the good news is that we can action small changes every day to turn around our resilience and take control of how we cope. As we commence another new year that is sure to try us, I have some tips for you.
Developing resilience involves maintaining flexibility and balance in your life as you deal with stressful situations and/or if your menopause symptoms are the cause of feeling stressed and over-whelmed.
We often don’t think of this time of our life as contributing to our stress levels, but as the relatively new Swiss research indicated, peri-menopause and menopause changes can really challenge our emotional and physical resilience.
The good news is that day by day we can move towards becoming resilient to whatever life throws at us. And undoubtedly, 2023 will have a lot to throw! So, with a focus on our health as we move through menopause, I thought I would share with you my top-tips for becoming more resilient in your menopause and post-menopause years:
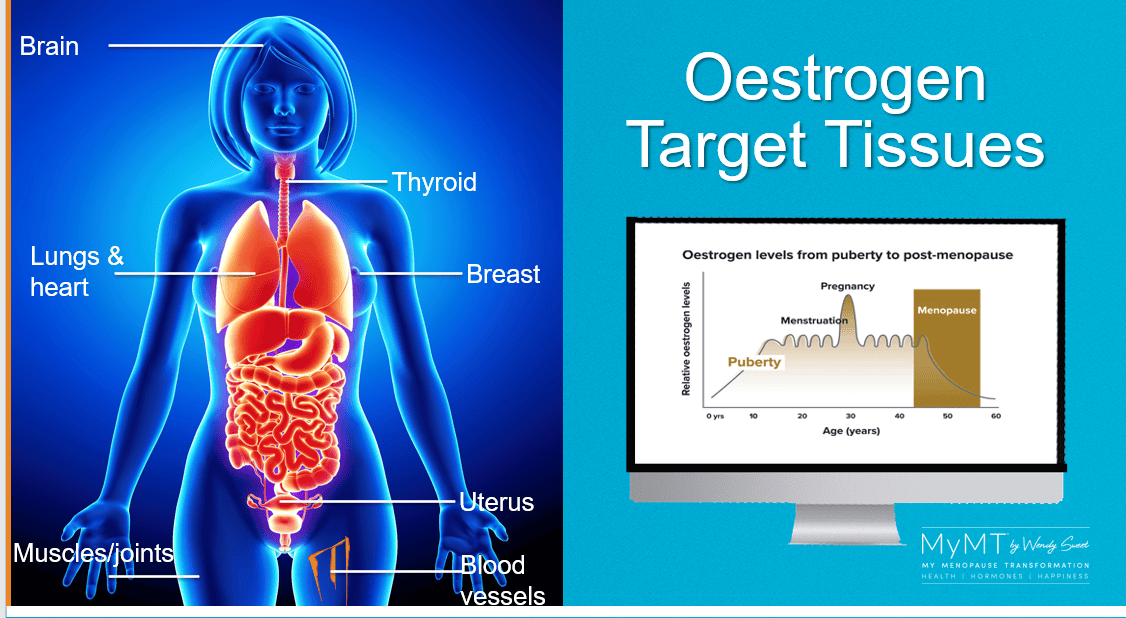
- Knowledge is power. Don’t just rely on your friends or family to explain menopause. Nor should you think of it as doom and gloom (although it often feels that way and many believe that it is because this is the dominant paradigm in medical circles). As the biological gateway to our ageing, our menopause symptoms become worse when we aren’t adapting well to this change in our life-course. So, for starters, have a listen to my Masterclass on Menopause. It might just help you have some ‘aha’ moments. When oestrogen levels decline, there are effects all around the body, not just in your ovaries!
2. Your menopause symptoms and/or weight gain are not insurmountable problems. There are lots of things you can do to manage these concerns. The first thing is to accept that your lifestyle needs are changing with age and how you respond to this is important. Going into denial doesn’t work! As well, you can change your nutrition, change your exercise and change your mindset to one of looking forward to feeling healthier with age. As I always mention, “don’t look back, because you aren’t going that way now!”

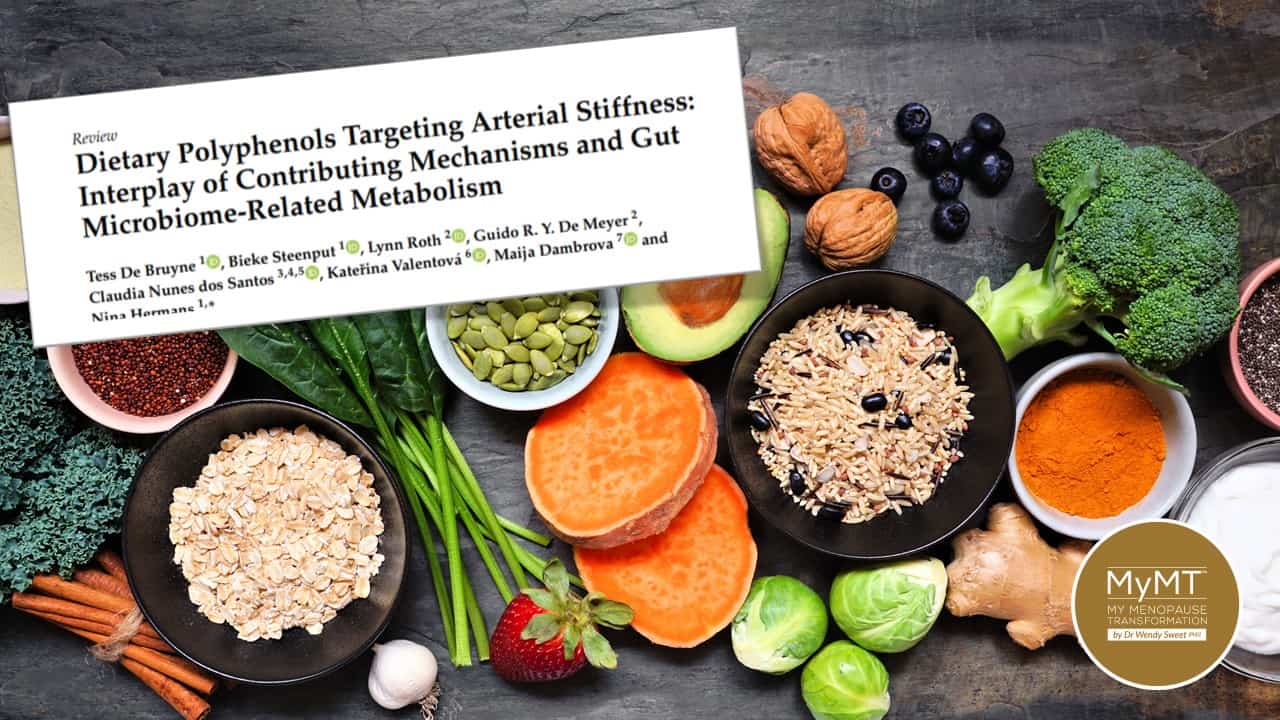
3. You need to sleep! Perimenopause is a difficult period in a woman’s life, disrupting her quality of life and sleep quality. As such research continues to support that this may lead to disturbances in eating behavior and body weight gain. Restoring your circadian rhythm is crucial as is changing when and what you eat in order for improved gut health.
The severity of menopause symptoms and the degree to which they interfere with the activity and quality of life varies among women and not sleeping has a major influence on our outlook doesn’t it?
But part of this conundrum sits with our changing gut health as we move through menopause. As oestrogen declines, we are more vulnerable to leaky gut syndrome and this is important as part of (re)building your immune and mental health resilience too.
This is why many of the supplements you may be buying in menopause, mainly have a probiotic effect on the gut (as well as offering anti-inflammatory effects) so your food intake is just as important to change too.
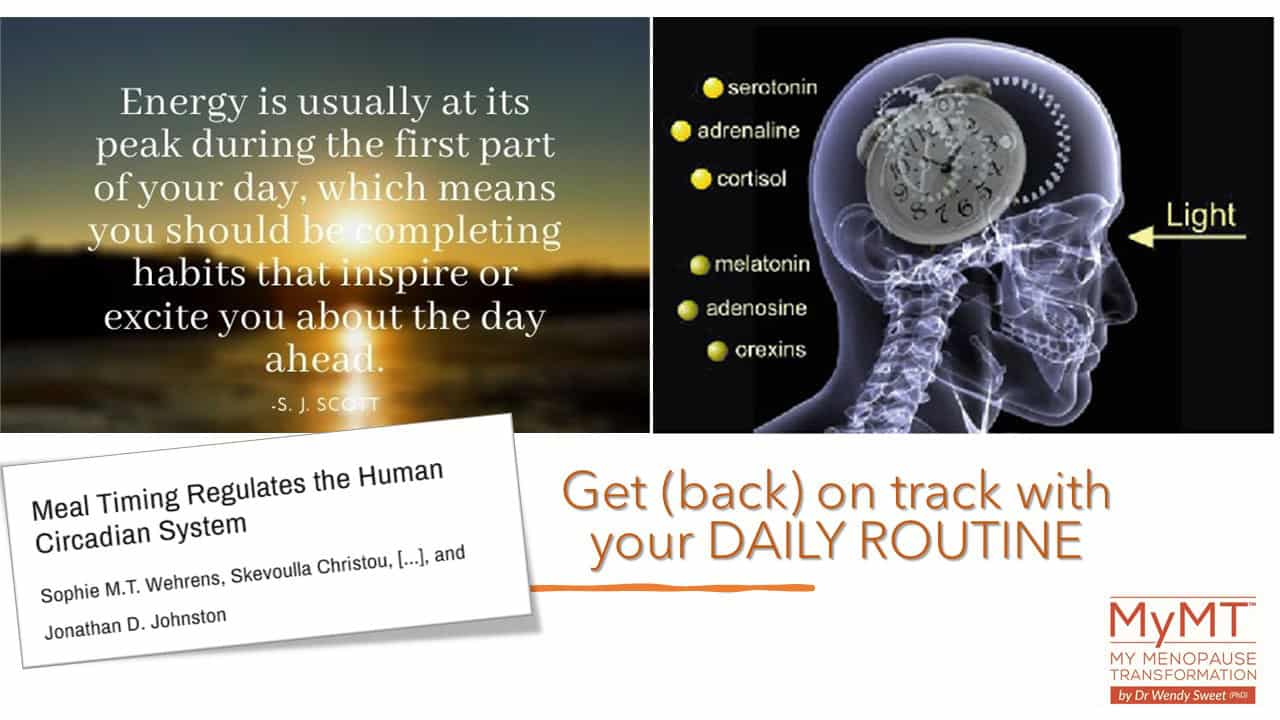
4. Re-balancing hormonal function requires a routine. I’ve been talking about this aspect of our health in the coaching group this week. I have thousands of women in this wonderful community who are re-establishing their routines after the holiday period or who are new to the programme because they’ve joined me on the Transform Me January sale.
My advice to them is always to restore a routine that can be maintained throughout the year. Mammalian circadian rhythms are driven by a master clock, within the suprachiasmatic nuclei (SCN) of the hypothalamus, and peripheral clocks located throughout the body. For the circadian system to function optimally, individual clocks must be correctly synchronized to one another and to the external environment.
5. Find exercise or activity that motivates you! As a sport and exercise researcher I cannot talk about resilience without talking about exercise! And you don’t need to exhaust yourself either – especially if you aren’t sleeping. If we are going to improve our resilience in 2022, then we have to find ways to move that energise us and don’t exhaust us. I talk a lot about this in my programmes. There is too much emphasis on high-intensity, athlete-driven exercise within fitness environments these days, but we don’t need this type of exercise to stay healthy.
We need exercise that is aerobic (to improve cardiac health) and yes, we need some strengthening and flexibility exercise too. But most of all we need to do exercise that improves our mental health, so find the exercise that you can sustain and that you enjoy and that gives you pleasure. Because without enjoyment and pleasure, then I know you won’t adhere to it! Nor will you be able to adhere to it if your joints are sore, so when you can, pop to the website and learn about my Joyful Joints Restoration module HERE (which is also in all of my programmes).

On a river, you know that you encounter different currents, rapids, slow water and shallows. We all know that it’s the same for ‘life’ and the changes you experience help to make you the unique individual that you are.
I know myself that when menopause arrived, it all got very confusing. So too does the weight gain and other symptoms that you may be experiencing as I did too. Hence, I hope that as we move into 2022, you can build your resilience to whatever the world and menopause still has to throw at you. There are numerous online resources as well as self-help books and support groups. As well as the support you get with MyMT™ – I love how women come on board for the knowledge, but stay for the connection and support.

Dr Wendy Sweet (PhD)/ Member: Australasian Society of Lifestyle Medicine.
References:
American Psychological Association (APA). The road to resilience. Online resource.
Azzeddine, S., Benharrat, L. et al (2021). Sleep quality and its relationship with climacteric symptoms and quality of life in women on menopausal transition. The North African Journal of Food and Nutrition Research. 5(12), 93-99.
Becker S., Manson J. (2020). Menopause, the gut microbiome, and weight gain: correlation or causation? Menopause. 28(3), 327-331.
Childs, E., & de Wit, H. (2014). Regular exercise is associated with emotional resilience to acute stress in healthy adults. Frontiers in physiology, 5, 161. https://doi.org/10.3389/fphys.2014.00161
Schmidt PJ, Murphy JH, Haq N, Rubinow DR, Danaceau MA. (2004). Stressful life events, personal losses, and perimenopause-related depression. Arch Womens Ment Heal. 7:19–26.
Soares C. (2017). Depression and menopause: current knowledge and clinical recommendations for a critical window. Psychiatr Clin North Am. 40:239–254.
Süss, H., Willi, J., Grub, J., & Ehlert, U. (2021). Psychosocial factors promoting resilience during the menopausal transition. Archives of women’s mental health, 24(2), 231–241. https://doi.org/10.1007/s00737-020-01055-7

