She emailed me from the UK. “My worst symptom is brain-fog” she mentioned. “I work at a computer all day and I’m feeling forgetful. I’m worried that I will get dementia as my mother did. I wonder if you have any solutions? I’m already on the Paleo diet and doing weight training.”
It wasn’t the first time I’ve had this type of email. It’s hard to explain to women that despite the hype about weight training and a high-protein and high-animal fat diet during menopause, for many women, this doesn’t suit their brain health and cognition.
Whilst I reminded this woman to check-in with her Doctor as she may be a candidate for hormonal therapy, I also explained that the best diet for brain health is not a high-protein nor a high-fat one. Nor is the best exercise for our brain health to perform daily weight training.
As many of your clients have returned to work over the past couple of months, I wonder how they may be getting on with their menopause symptoms, including brain-fog, memory problems and of course, anxiety, even though they may already be on HRT?
Menopause at work is getting a lot of publicity these days, which is heartening, however, there are strategies that you can share with them, if they are forgetful. I share my top-5 with you below.
Symptoms such as forgetfulness, fuzzy head, anxiety and inability to think properly affect numerous women during menopause. Whilst I’ve talked about these symptoms in the past, I want to remind you of the lifestyle solutions that you can be putting into place.
The changes in oestrogen levels during menopause are associated with the occurrence of menopausal symptoms and cognitive (mental) decline. Indeed, these fluctuations have a significant impact on the whole body, including the central nervous system, and can be responsible for changes in our cognition (thinking and processing information) and our mood. (Hara, Waters et al, 2015).
Some of your clients may also be experiencing symptoms from long-covid, which, when it comes to brain fog, is a double-whammy for women in midlife.
With millions of women globally entering into their menopause transition, scientists are now catching up on research into menopause brain-fog and memory problems.
This is partly because Dementia and Alzheimer’s Disease in older age, is a growing pandemic (Heneghan, Deng et al, 2022), which as many of us already know from looking after ageing parents, is a health condition that presents profound challenges to health care systems, families and societies throughout the world.
Numerous women complain of forgetfulness around the time of the menopausal transition and because of the association between episodic memory loss and Alzheimer’s disease, this ‘forgetfulness’ symptom (aka brain fog) is of course worrisome.
However, forgetfulness is a common symptom at other ages too, especially during puberty and pregnancy – both of which are stages of life whereby there’s a bit of chaos with hormones, particularly oestrogen and progesterone.
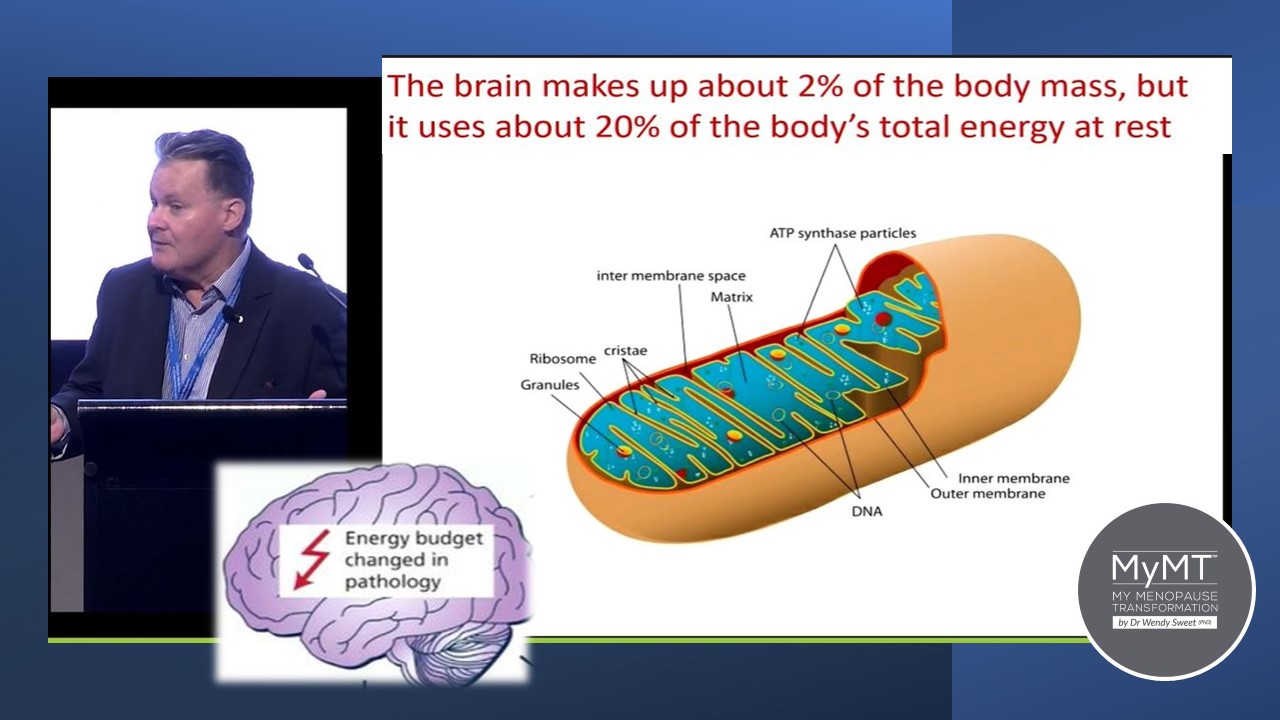
Professor Zoltan Sarnyai (that’s him in the image below) is a neuroscientist researching mental illness at the Laboratory of Psychiatric Neuroscience at James Cook University in Australia. He’s a very clever guy.
It was his presentation that bought my attention to the link between menopause hormonal changes, brain-fog, stress levels and the mitochondria. Considering that mitochondria are involved in a multitude of cellular processes, mitochondrial dysfunction has been shown to play a role within several age-related
diseases, including cancers, diabetes (type 2), and more recently, neurodegenerative diseases. (Bartman et al, 2024).
With this emerging knowledge about the link between brain mitochondria and mental health and cognition, don’t you think it makes sense to understand the lifestyle solutions that are evidenced to improve brain mitochondrial function with ageing and share these with your clients? I hope so!
The link between mitochondria, menopause and your brain health
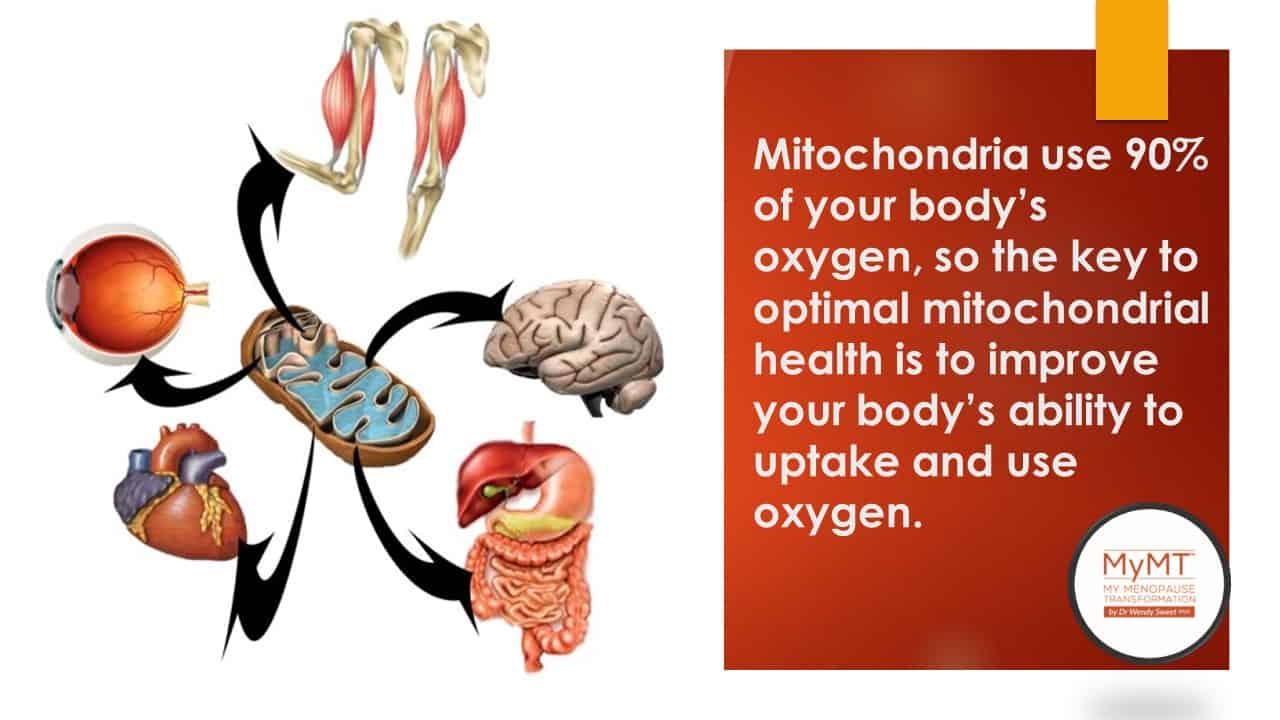
Mitochondrial cells are where energy is made. There are millions of mitochondrial cells around the body. They have multiple and crucial roles in cell maintenance, survival and wellbeing.
Mitochondrial dysfunction is one of the primary hallmarks of ageing and is implicated in several age-related diseases, mentions new research on mitochondria and brain ageing (Bartman et al., 2024). These diseases include different forms of cancer, diabetes (type 2), and neurodegenerative diseases.
One of the most popular theories of ageing that I mention in my CPD Health Practitioner Course, is also about ‘The Mitochondrial Theory of Ageing”, first postulated by Denham Harman 50 years ago. As explained in Bartman et al. (2024) paper, this theory postulates that ageing is the result of accumulative damage caused by free radicals generated by metabolic reactions or as by-products of cellular processes. Over time, this damage impacts the function of body organs, including the brain.
My interest in this theory of ageing, as well as others, was piqued when I completed my women’s health and ageing studies, and from that point on, I have positioned the menopause transition in women’s ageing studies.
Mitochondria also play an essential role in the generation of steroid hormones including the female sex hormones. As such, female sex hormones are, in turn, able to modulate mitochondrial activities. (Lejri et al. 2018).
We already know that a large amount of oestrogen in the female body is released from the ovaries. But as it’s released, it circulates throughout the body and crosses the blood-brain barrier to act upon the cells within the brain. In the brain, oestrogen has a number of roles including helping with cerebral blood flow as well as in the preservation and maintenance of nerve transmission. Oestrogen also operates as an anti-inflammatory agent in the brain.
This is why, as levels of oestrogen decline during menopause, this stage of our life becomes a perfect storm for disruptions to brain function and cognition. Oestrogen acts directly upon mitochondria in the brain. (Del Río et al., 2018). It makes sense then, that as women move through menopause, their brain mitochondria are affected in ways that promotes inflammation.
This is backed up in dementia studies whereby growing evidence suggests that up to 40% of all dementia cases are associated with known pro-inflammatory lifestyle related modifiable risk factors, such as alcohol consumption, obesity, and hypertension among others (Heneghan, Deng et al, 2022) and that exposure to most of these risk factors begins a few decades before the onset of dementia.
It’s why I’m always telling you to tell your clients, that their midlife years matter! From dementia to cardiovascular disease to obesity-related health concerns, the midlife years present a critical and unique window for disease-altering interventions.
Age, stress and other factors such as menopause hormonal changes disrupt the role of the mitochondria and may impact inflammatory changes in brain neurons (nerves). The rate of this change is dependent on your client’s lifestyle – past and present.
It’s no surprise that during our entry into peri-menopause, the stage before periods end, increases the incidence of forgetfulness and brain-fog.
However, as Professor Sarnyai reminds us, stress (both current and past), has a long-lasting and negative impact on brain mitochondria.
Chronic stress causes an increase in inflammation in mitochondrial cells. Then these inflammatory changes may lead to a number of symptoms, your client may be experiencing, including:
- fatigue
- brain fog and depression
- memory loss, lack of motivation and feelings of over-whelm
- pain and soreness in muscles
- headaches and migraines
- poor sleep
Do any of these symptoms sound familiar to you?
Make Changes to your Lifestyle to Reduce Brain-Fog
1. Stay stimulated! Lifestyle has a multipronged impact on cognition and the brain. In Heneghan’s new study, the research team reported several lifestyle activities as protecting brain health and cognition in later life. This included frequent engagement in physical, social and intellectually stimulating activities. This includes aerobic exercise. Exercising aerobically whereby you aren’t completely out of breath, helps your brain health.
Aerobic exercise has numerous biological and psychological effects, such as increasing the gray matter volume in the frontal and hippocampal regions; inducing the release of positive brain hormones; enhancing the connection between brain nerves and improving the function of cerebrovascular vessels along with increasing blood flow with more oxygen and nutrition to brain centres. (Elsayed et al, 2022). These effects are not the same when lifting heavy weights.
I talk a lot about this in my 12 week Rebuild My Fitness programme as well as my Circuit Breaker and Transform Me programmes.

2. Change your diet to the MIND diet. Numerous studies on the health of older women now promote the Mediterranean Diet, as I do in my 12 week programmes as well (I’ve adapted the nutrients specific to menopause and menopause weight loss). But the “Mediterranean-DASH Intervention for Neurodegenerative Delay” (MIND) diet, goes one step further. If you are concerned about dementia and your ever-present brain-fog, then the MIND-study shows that subjects lowered the risk of Alzheimer’s Disease by as much as 53 percent in participants who adhered to the diet rigorously, and by about 35 percent in those who followed it moderately well. [Arjmand, 2022; Morris et al, 2015]
3. Exercise and Mindfulness help to boost glutamate production in the brain. 80% of all nerves in the brain need glutamate in order to transmit nerve impulses but chronic stress negatively impacts glutamate production. Glutamate is important to memory, cognition, and mood regulation and both exercise and mindfulness have a strong impact on brain glutamate levels. (Pal, 2021).
4. Sleep all night! Without enough sleep, our mitochondria don’t produce enough energy. Learning the specific steps to turning around your client’s sleep is a key teaching in the CPD Practitioner Course too. This includes, understanding why their Vitamin D levels are a key component of their brain function and mitochondrial function.
5. Lose excess weight. Obesity is known to have a negative impact on cardiovascular and metabolic health, but it also impacts brain structure and function. Whilst this is known to be linked to gut health changes, if women are overweight or obese, then gray and white matter may increase in inflammatory changes, thus impacting decreased cognitive function. (Olsthoorn et al, 2021). How to achieve this with your midlife clients who are overweight, is in the certified Menopause Weight Loss Coach Course.
Whilst millions of women find relief from their brain fog and mood swings with oestrogen replacement medications and/or anti-depressants, it is known that there seems to be a window of opportunity in peri-menopause to take Menopause-HRT. Hence, for your older clients who may not be able to take HRT, helping them to make changes to their lifestyle to help maintain healthy mitochondria is an important coaching strategy.
Numerous changes occurring around the body are perfectly normal, including changes to the mitochondria and brain neurons as women age, but what their focus should be on, is to slow down this rate of change. That’s why understanding the specific lifestyle changes are crucial to helping your clients manage their health in midlife and in post-menopause.
How to achieve this with your clients is in my Health Practitioner Courses. I hope you can join me sometime.
Dr Wendy Sweet (PhD)/ Member: Australasian Society of Lifestyle Medicine

References:
Arjmand, G., Abbas-Zadeh, M. & Eftekhari, M.H. Effect of MIND diet intervention on cognitive performance and brain structure in healthy obese women: a randomized controlled trial. Sci Rep 12, 2871 (2022).
Bartman, S., Coppotelli, G., & Ross, J. Mitochondrial Dysfunction: A Key Player in Brain Aging and Diseases. Curr. Issues Mol. Biol. 2024, 46(3), 1987-2026; https://doi.org/10.3390/cimb46030130
Elsayed MM, Rabiee A, El Refaye GE, Elsisi HF. Aerobic Exercise with Mediterranean-DASH Intervention for Neurodegenerative Delay Diet Promotes Brain Cells’ Longevity despite Sex Hormone Deficiency in Postmenopausal Women: A Randomized Controlled Trial. Oxid Med Cell Longev. 2022 Apr 4;2022:4146742.
Filler, K., Lyon, D., Bennett, J., McCain, N., Elswick, R., Lukkahatai, N., & Saligan, L. N. (2014). Association of Mitochondrial Dysfunction and Fatigue: A Review of the Literature. BBA clinical, 1, 12–23. https://doi.org/10.1016/j.bbacli.2014.04.001
Hara Y, Waters EM, McEwen BS, Morrison JH. Estrogen Effects on Cognitive and Synaptic Health Over the Lifecourse. Physiol Rev. 2015 Jul;95(3):785-807.
Henderson, V. W., & Brinton, R. D. (2010). Menopause and mitochondria: windows into estrogen effects on Alzheimer’s disease risk and therapy. Progress in brain research, 182, 77–96. https://doi.org/10.1016/S0079-6123(10)82003-5
Heneghan A, Deng F, Wells K, Ritchie K, Muniz-Terrera G, Ritchie CW, Lawlor B, Naci L. Modifiable Lifestyle Activities Affect Cognition in Cognitively Healthy Middle-Aged Individuals at Risk for Late-Life Alzheimer’s Disease. J Alzheimers Dis. 2022 Dec 5. doi: 10.3233/JAD-220267.
Kwon, D. (2021). Could Mitochondria Be the Key to a Healthy Brain? Scientific American. Publ. June 18th, 2021.
Lejri, I., Grimm, A., & Eckert, A. (2018). Mitochondria, Estrogen and Female Brain Aging. Frontiers in aging neuroscience, 10, 124. https://doi.org/10.3389/fnagi.2018.00124
Morris MC, Tangney CC, Wang Y, Sacks FM, Barnes LL, Bennett DA, Aggarwal NT. MIND diet slows cognitive decline with aging. Alzheimers Dement. 2015 Sep;11(9):1015-22.
Olsthoorn L., Vreeken D., Kiliaan A. (2021). Gut Microbiome, Inflammation, and Cerebrovascular Function: Link Between Obesity and Cognition. Frontiers in Neuroscience, (15), 1-13.

