Women’s health and ageing research is replete with cardiovascular disease studies. The declining health of our mother’s generation have paved the way for this type of research in older women. For many women, menopause is the start of their changing heart health … but here’s the thing that our mother’s generation didn’t know – it doesn’t have to be this way.
Menopause is the time of our lives when we are most at risk of high blood pressure and changing heart health and researchers now understand that our mid-life years are the time to change how we look after ourselves. Otherwise, hot flushes, poor sleep and aching joints continue into the post-menopause years.
With women’s death rate from heart disease in America nearly eight times higher than death rates from cancer and New Zealand, Australia and the UK leading the world in heart disease incidence, increasing evidence indicates that hormonal changes in menopause may also be involved (Maas, 2020).
Over 30 years ago in the early 1990’s, when I was a former ICU nurse, every now and again, there would be a call to go and help-out the busy nurses in the Coronary Care Unit. At the time, I didn’t give a thought to how many of the patients lying in beds hooked up to cardiac monitors were women who had just arrived in menopause or post-menopause.
But they were – and now that I’m in post-menopause myself and with my women’s healthy ageing studies leading me down the rabbit-hole about how the effect declining oestrogen has on other organs around the body, including cardiac muscle and blood vessels, these memories make sense.
Women in their menopause transition and those already in post-menopause are at increased risk for changing heart health as they age. Whilst both weight gain and poor sleep patterns affect post-menopause heart health, new research reports why magnesium exerts a powerful influence on our heart health too.
At the time that I was helping out my colleagues in the CCU all those years ago, over 153,000 post-menopausal women in America were entering one of the largest women’s health studies to be undertaken. Today I thank them.
As participants in the Women’s Health Initiative Study they were recruited between 1993 and 1998 and their magnesium intake at the time, was assessed using a validated food frequency questionnaire.
It is well known that magnesium plays an important role in cardiac physiology, helping the heart to contract. Over the next decade, coronary heart disease was measured in this cohort as well as sudden death. Earlier this year, a brand new women’s health study has gone back to this original research, reminding us that as we move into our post-menopause years, [when our periods have stopped for a year or more], having adequate dietary magnesium (not supplements) matters.
When I present my live Masterclass on Menopause seminars, (now available online), I often asked women if they were taking lots of supplements. Most were. When I used to follow this query up by enquiring if they know if they work, most weren’t sure. This was my curiosity too.
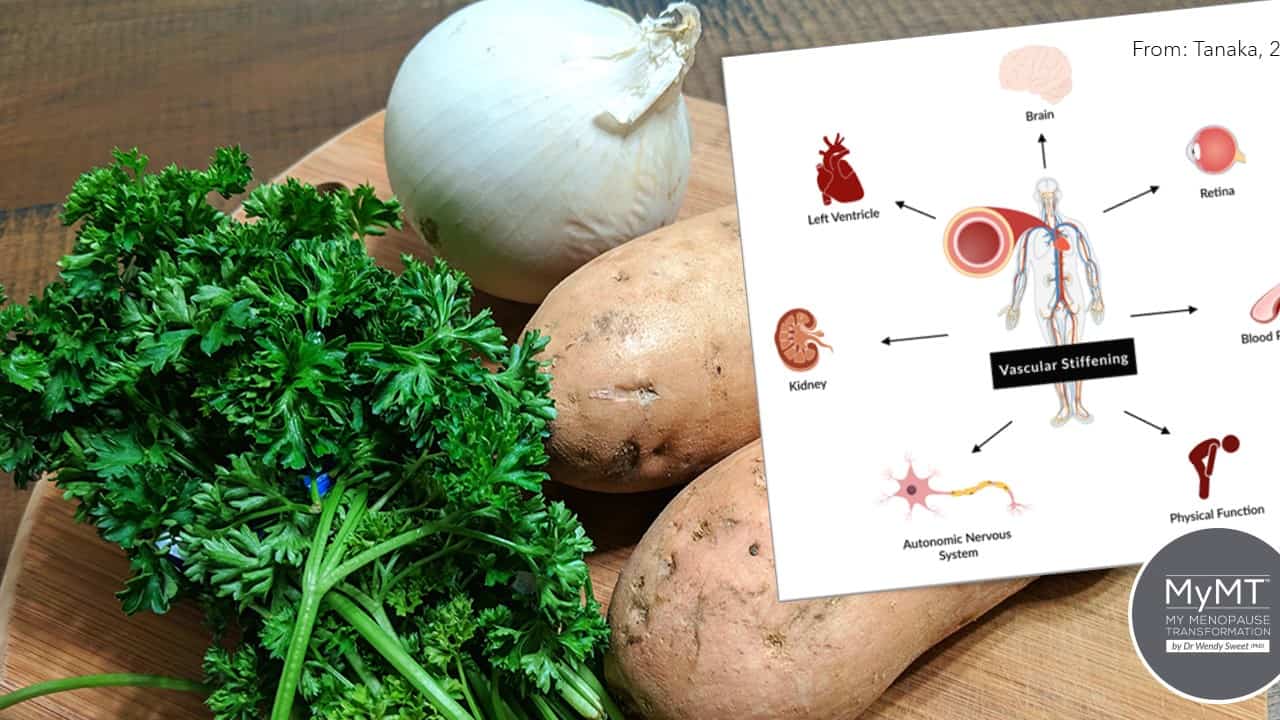
Vascular stiffness in blood vessels
Menopause is the gateway to our biological ageing. As such, there are changes to our blood vessels and other organs. In an age whereby media and pharmaceutical companies focus on marketing botox and other external products to promote anti-ageing, the salient point of our internal cellular ageing gets forgotten.
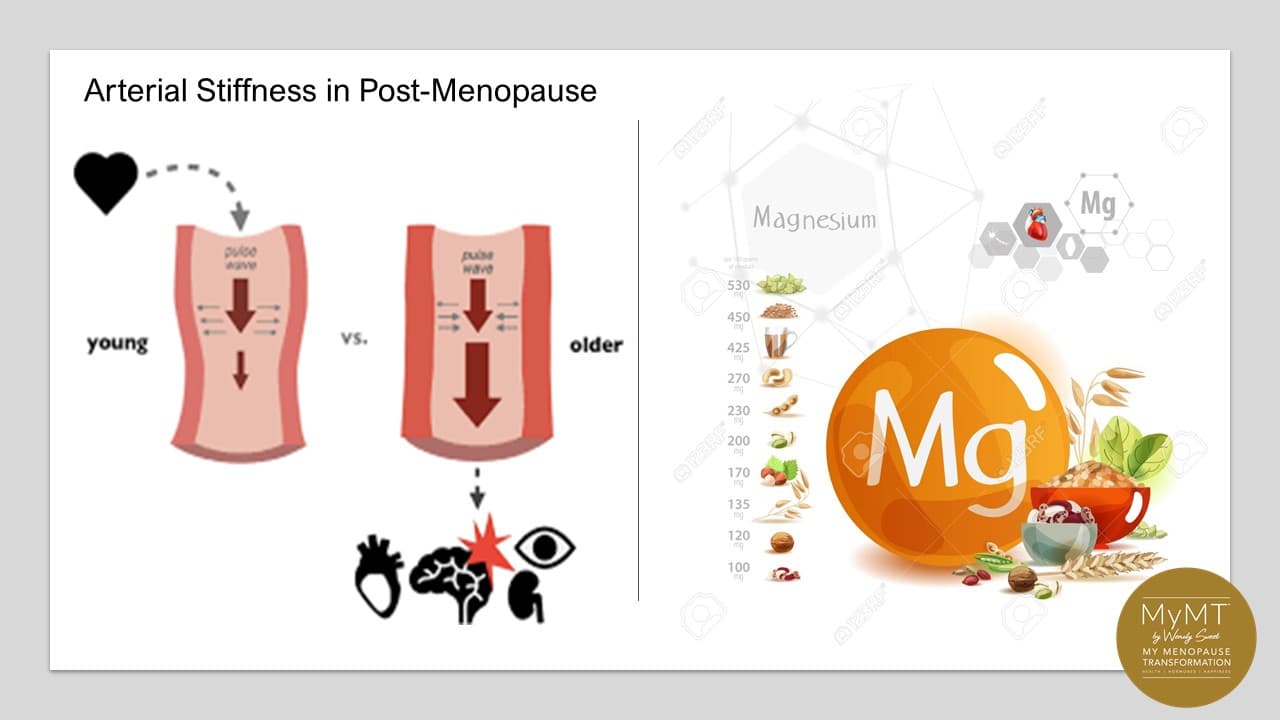
When menopause arrives, there are numerous structural changes that occur in our body, not just changes to our oestrogen and progesterone levels. This is an important point for all women, not only those who are regular exercisers. As we lose oestrogen, our blood vessels are ageing and this leads to vascular or arterial stiffness. The loss of elasticity in blood vessels and lymphatic vessels, means that we may may feel more bloated, our legs may feel heavy, restless and aching (especially for exercisers) and our blood pressure and heat regulation may get out of balance too. When we have busy, active lives, the vascular stiffness leaves us feeling exhausted.
These internal changes going on ‘inside’ our body are important for all of us to understand.With vascular stiffness arriving in mid-life and beyond, the risk of cardiac disease as we age increases. As such, one of the strategies that I promote in the MyMT™ programmes is to get women thinking about the magic of magnesium. Australia’s women’s health expert, Dr Sandra Cabot, values it as important too,
“To have a mineral found in nature, a mineral your body needs, a mineral that is easily and cheaply available (in pill or powder form) and known to be useful in treating or preventing dozens of medical conditions – to me, that sounds like a dream come true.” [Cabot, S. (2004). Magnesium the Miracle Mineral. SCB International Inc.

Why you may need Magnesium in Menopause:
Magnesium supplements have sky-rocketed over the past decade or so as they are heavily marketed to women in their menopause transition as the panacea for hot flushes, night sweats and other aches and pains. But there is another important role for magnesium in menopause too. And that is to help reduce our risk of heart disease and to regulate our blood pressure.
New research indicates that for women during menopause, magnesium is an important co-factor (helper) mineral for a number of enzyme functions that work specifically in cardiac mitochondria. And with my eye on our cardiac health as we age and go into post-menopause, there’s never been a better reason than menopause, to have a little re-think and focus on magnesium!
Magnesium is important for healing and so too, is it’s opposing partner, calcium. The two help to balance and restore muscle and nerve function in the body and help in a heap of other reactions in the body during and after menopause as well. Crucial for women who are busy and active, as Patricia is over there in Canada, as you can see in the banner below.
We need around 320mg to 400mg daily of magnesium and preferably from our diet. As an ‘essential mineral’ this means that our body doesn’t make it. With magnesium involved in more than 300 enzymatic reactions involving energy metabolism and blood pressure regulation, it is pretty important to our health and energy. For us girls going through menopause, it is also important for:
- helping hormones to bind to receptor cells
- the prevention of too much calcium getting into cells
- muscle contraction and nerve activity (along with calcium)
- control of blood vessel dilation and tone
- helping nerve impulses to pass through cardiac muscle.
But perhaps the most important issue, is that magnesium deficiency has been shown to play a role in inflammation and when our body is stressed (as it is when we aren’t sleeping in menopause), then magnesium deficiency also leads to an exaggerated response to even more stress, especially in our cells and tissues, through our nerve-hormonal pathways.
This type of stress is called oxidative stress and makes our hot flushes, muscle and joint pain and weight gain become worse during menopause and when we move into post-menopause, especially if women are regular exercisers.

Why might we become low in magnesium?
Several factors can cause low magnesium. Top of my list, would be an unhealthy liver or gut. If we have inflammation in these organs, then any magnesium that we do have in our diet, cannot be absorbed properly.
Many women don’t have ideal gut health to absorb as much magnesium as their body needs. It’s why for my APRIL MyMT™ ProgrammeSale, I’ve included a bonus Gut Heaalth module, along with my brand new Heart Health module and a Joint Health Module.
Next on my list is doing too much exercise or experiencing high stress levels. When this occurs and we are always in ‘fight or flight’ mode, then our lovely long vagus nerve is always stimulated. This increases gut motility or movement, and when this happens, again, the food passes through our gut too quickly, so absorption time is delayed.
When it comes to exercise, magnesium matters. In aerobic exercise, higher intake of Mg has been shown to be associated with less oxygen needs and better cardiorespiratory outcomes (Zhang et al., 2017) – something that all of you who are active need to know.
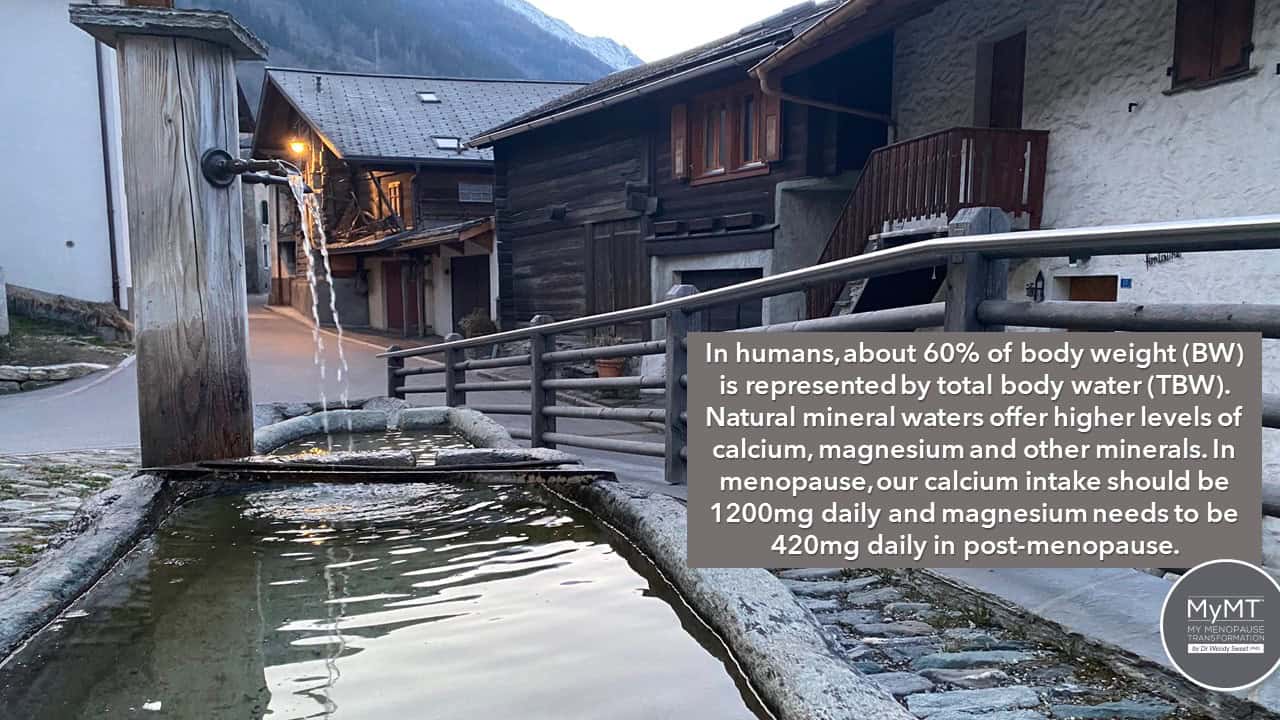
Studies have also shown that the quality of our food and food processing means that magnesium can be deficient in our diet, but alcohol can decrease magnesium uptake as can osteoporosis medication as well as poor water levels of magnesium.
The significance of magnesium and its relationship to the origin of life has been traced by researchers interested in the body’s dependence on it. In their 1999 review article on magnesium, Fawcett, Haxby & Male contend,
“The importance of magnesium is derived from the composition of the earth’s crust (rich in iron–magnesium silicate) and the primeval ocean rich in magnesium, to the formation of chlorophyll with magnesium at the centre of the molecule, and finally to its incorporation into the animal cell containing adenosine triphosphate (ATP) with its dependence on magnesium.”
When magnesium levels get low, then we can experience leg cramps, increased muscle twitching and cardiac palpitations. With these all noted symptoms of menopause hormonal changes, then yes, maybe we do need to look at our magnesium levels every so often.

There are some great ways we can improve magnesium uptake during menopause:
- Epsom Salts: Magnesium has been used as a therapeutic agent for hundreds of years and well before pharmaceutical companies sold magnesium to us in bottles! Magnesium-rich waters of Epsom Spa Town have been known to be beneficial ever since the 16th Century (this is where Epsom Salts were discovered).
- Food Sources: If you want to use your diet to increase magnesium rather than supplements, then get more beans, nuts and whole grains into you. For my amazing women on the MyMT™ programmes, I get them to increase their intake of organic brown rice, green leafy vegetables and they can also have bananas, dark chocolate and of course, a black coffee – all foods and drinks which are rich sources of magnesium and other healthy nutrients.
- Artesian Water: When I was in Switzerland earlier this year after two years of our borders closing, it was so nice to taste again, the mineral-rich water in the small village I was visiting. I had almost forgotten how wonderful it was. Everywhere in the village, troughs were brimming over with glacial water coming down from the Swiss Alps. In my visits there in the past, I learnt that the ‘magic’ of these waters lay in the richness of two minerals – calcium and magnesium. Further investigation and local knowledge, led me to discover that just 1 litre of this beautiful alpine water delivers around 50% of the daily requirements of calcium and magnesium to drinkers. No wonder I was told that many locals live to a ripe old age! Women from around the world who are in my coaching groups get all this fabulous knowledge as well.
Magnesium is a vital tool in our dietary tool-box as we transition through menopause as are most minerals and vitamins. But if we aren’t absorbing these nutrients then the priority is to turn around the gut, liver and cardiac inflammation that prevents magnificent magnesium from doing its job. I show you how to do this in my 12 week programmes and it’s why I’ve bundled up these modules in both of my foundation programmes (Circuit Breaker for thinner women and Transform Me for overweight women) this month. If you are in post-menopause and your symptoms are troubling you still, then I hope you can join me.
Sometimes we do need a boost from supplements, but other times we can get adequate amounts from improving our focus on the right foods at different life stages.
As I say to each and every one of the women in the MyMT™ Community,
“When it comes to our menopause transition and as we step into our post-menopause years, you don’t need a lot of food, just the right food. That includes the right food for your heart health as you transition menopause – this aspect of our nutrition as we age is being forgotten in a world of unhealthy and not-so-well evidenced dietary claims, many of which don’t focus on women going through menopause.”
[Dr Wendy Sweet, PhD/ Member: Australasian Society of Lifestyle Medicine].
References:
Li, J., Hovey, K. et al. (2020). Association of dietary magnesium intake with fatal coronary heart disease and sudden cardiac death. Journal of Women’s Health, 29(1), 1-6.
Lorenzo, I., Serra-Prat, M., & Yébenes, J. C. (2019). The Role of Water Homeostasis in Muscle Function and Frailty: A Review. Nutrients, 11(8), 1857. https://doi.org/10.3390/nu11081857
Schuchardt, J. P., & Hahn, A. (2017). Intestinal Absorption and Factors Influencing Bioavailability of Magnesium-An Update. Current nutrition and food science, 13(4), 260–278. https://doi.org/10.2174/1573401313666170427162740
Zhang, Y., Xun, P., Wang, R., Mao, L., & He, K. (2017). Can Magnesium Enhance Exercise Performance?. Nutrients, 9(9), 946. https://doi.org/10.3390/nu9090946

