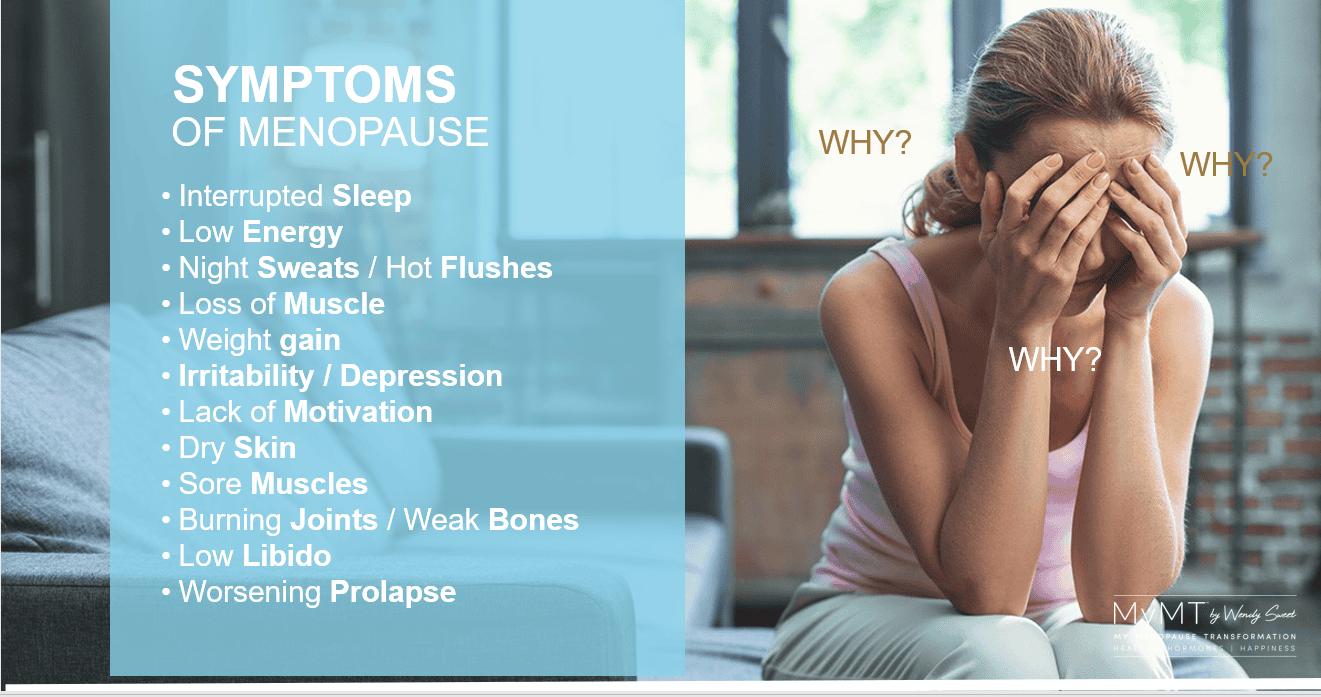
Why do we have so many symptoms that impact on how we feel during our menopause transition? Why do we all need to suddenly take supplements and medicines when we’ve been healthy all our lives? Why can’t we sleep? Why can’t I control my weight gain?
And why can’t we tolerate doing the exercise that we love to do? WHY? WHY? WHY?
If you’ve ever had these thoughts, then you aren’t alone. I used to ask myself these questions too.
The symptoms of menopause are numerous and there’s a reason for this. A woman’s menopause transition is the gateway to the next stage of her life – her post-menopause years, and as such, our declining reproductive hormones, affect organs and tissues around the body.
I didn’t understand this when I went into my own menopause transition, as the hallmark symptoms of menopause were considered to be hot flushes/flashes, brain fog and anxiety. None of the other symptoms were even mentioned.
As a university-level lecturer in physiology and sports science, my doctoral research on women’s healthy ageing and exercise, led me down the menopause-symptom rabbit-hole.
Midlife is a time of life that many women find that their tolerance to exercise changes. According to much of the physical activity participation research, most women also give up exercising in mid-life (Arigo et al, 2022). I now understand why.
When sleep evades you night after night and your joints and muscles are sore, the last thing you feel like doing is exercising for your health. Many of my research participants found this, as do women on my lifestyle-change programmes.

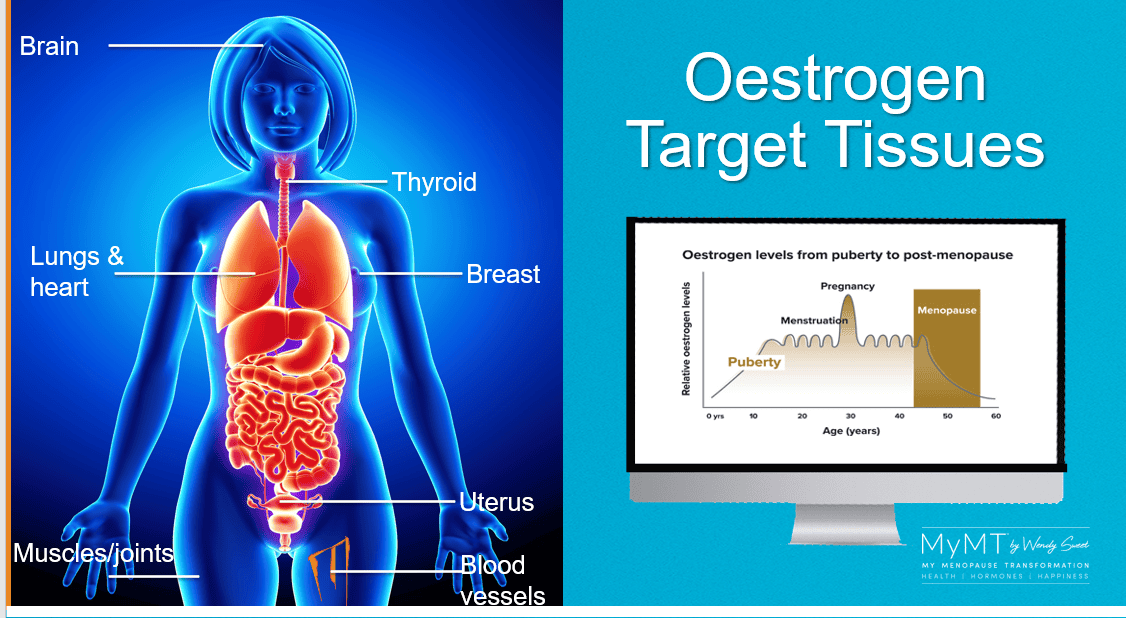
As I began to put menopause into the context of our biological ageing and the fact that all of our hormones work together in the body, I also learnt that we have oestrogen receptors around our body – especially in our brain, skin, muscles, tendons, cardiac muscle, blood vessels and fat cells.
This helps to explain why many women experience so much symptom chaos that they don’t attribute to menopause. Positioning our menopause transition in ageing research, enabled and empowered me to look at my own symptoms in more depth.
The role of inflammation in many diseases of older age, especially with regard to cardiac health for women, is important in this context.
Our symptoms can be so confusing, can’t they? But no matter what treatment considerations you explore, our understanding of why we are experiencing these symptoms is a great start for you, no matter what stage of menopause you are in – perimenopause, menopause or post-menopause.
So, read on to discover my top 5 reasons for your symptom chaos and/or weight gain as you move through this important stage of life.
My 5 reasons for your symptom chaos and/or weight gain during menopause:
- Your changing liver health: When oestrogen production begins to decline in peri-menopause, the two ‘master hormones’ which are produced in your pituitary gland [Luteinising Hormone and Follicle-stimulating Hormone], are still trying to send signals to the ovaries to increase production of oestrogen. However, ovarian oestrogen receptors are ageing and dying off, so the nervous and hormonal system can get out of balance.
When women have a lot of stress in their life, or they aren’t sleeping, oestrogen can decline more rapidly and some of the signals between the brain and the ovaries get out of balance (one of the reasons that Menopause HRT can be effective in helping to reduce anxiety and improve memory as it helps to slow down the rate of this decline).
But there is another factor as well, and that is, the knowledge that perimenopause is an inflammatory event and there are changes in other organs due to ageing (‘inflammaging’), including the liver and gut.
If the liver is inflamed, then it may not be able to metabolise oestrogens effectively. And remember that despite the hormonal decline in oestrogen, we also have oestrogens in our food, chemicals, pollutants and of course, alcohol is metabolised into types of oestrogens too. For those of you struggling with your weight, these ‘other’ sources of oestrogens can be transported to fat cells when the liver is inflamed.
Fat cells store these additional oestrogenic compounds as we move through menopause and for women who may be overweight, the fat cells are now known to produce their own oestradiol.
Hence, oestrogen storage in fat cells cause them to expand and oestrogen can become the ‘dominant’ hormone in relation to it’s opposing hormone, progesterone.
I’ve written about this before as it’s a condition called ‘oestrogen dominance’ and you can read the full article HERE.

- Lowered Progesterone: For those of you who aren’t overweight, don’t forget that high stress levels or insomnia can contribute to lowered progesterone. If you aren’t sleeping, then your stress hormone cortisol not only remains elevated overnight, but can also remain chronically elevated.
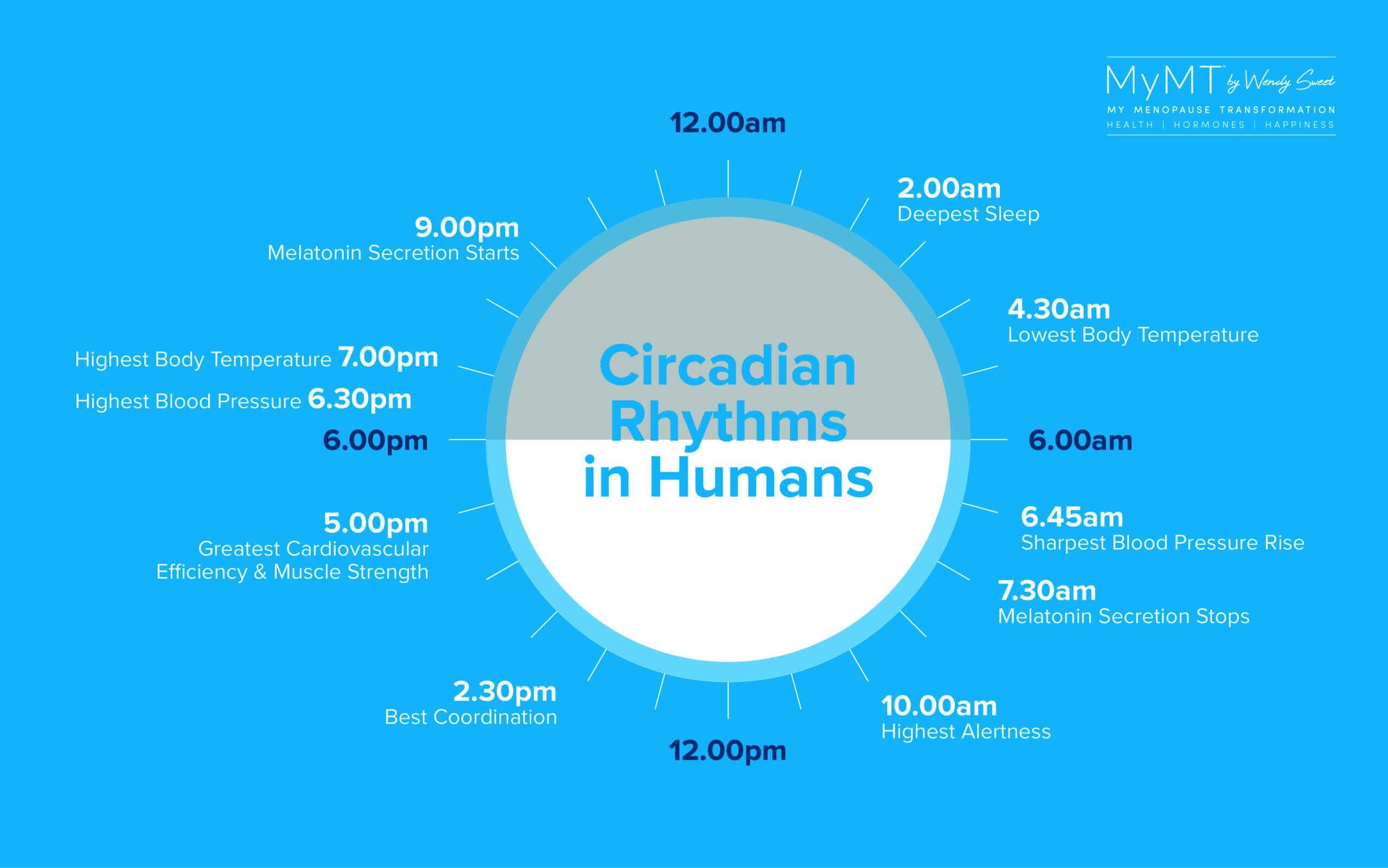
When the body needs to continue to produce the chronic stress hormone cortisol, and the circadian (day/night) rhythm is out of balance, then the pituitary gland in the brain and the adrenal glands use up greater amounts of cholesterol in order to make pregnenolone (a precursor to progesterone) and convert this to cortisol. However, that’s only part of the story.
In sports science research, an over-stressed and over-trained female athlete, often presents with disrupted menstrual cycles. This is because the two master hormones, FSH and LH, are reduced in production. This is a female survival mechanism, as in times of stress, reproductive function is preserved.
This is often called ‘pregnenolone steal’ however, as science has moved on, it’s a complex process! I often talk about this in my seminars and refer to women who may be doing a lot of exercise. Again, too much physical exercise can be a source of stress for some women.

- Disrupted thyroid, adrenal and pituitary hormones. In women, the Hypothalamus-Pituitary-Adrenal-Thyroid Axis is powerful.
The HPA-Thyroid Axis connects the brain with the adrenal glands. What this means in menopause, is that if our pituitary gland (which is controlled by the hypothalamus) is not functioning effectively, then this can increase feelings of anxiety, memory loss and stress.
The way to manage the HPA-Thyroid Axis is through improving the optimal function of the pineal gland – which controls your circadian rhythm. (Hirotsu et al, 2015). This is why the very first module you listen to in my 12 week programmes is simply called ‘Sleep All Night’. It’s that important. Especially for those of you wanting to reduce your anxiety, reduce inflammation, improve brain-fog, rebalance your hormones and for some of you, lose weight.
- Lowered Vitamin D levels. Our skin is our largest organ and is full of oestrogen receptors. Vitamin D is a fat-soluble vitamin and is produced in the skin with the help of oestrogen.
Therefore, many women are at risk of low vitamin D levels and because Vitamin D is now recognised as a hormone, low levels have an effect on other hormones in the body too.
When Vitamin D is low, hot flushes are increased and memory loss/ foggy brain may become worse. Vitamin D is involved in the production of calcium and our bones and muscles require calcium to help them to remain strong.
Vitamin D is such a powerful hormone for women to monitor in menopause because it is also implicated in melatonin production, which is our sleep hormone. When Vitamin D levels are low, our insomnia increases and serotonin production is reduced, contributing to worsening mood swings and depression.

- Increased inflammation. My most important message to women is that worsening menopause symptoms are not only due to our changing hormones as we age, but they can become worse due to the build-up of inflammation in the liver, gut, muscles (including cardiac muscle) and blood vessels.
Don’t forget that over the past four decades, we’ve been the ‘guinea-pig’ generation for processed foods, medicines, chemicals, high impact sport and exercise and other pollutants, which have led to cellular changes in our cells and tissues. This is seen through the relatively new science of epigenetics.
By the time menopause arrives, much of this ‘invisible’ inflammation is switched on as our hormonal environment changes with age. That’s why, to turn around our symptoms, we have to reduce the effects of this inflammation. Yes, it can be done!

When we start to change our lifestyle to accommodate the changes occurring as we we move through menopause, we can begin to restore balance in the body. As such I focus you on 3 phases of health transformation as you progress through the MyMT™ programmes over 3 months.
(a) Reducing inflammation that’s been building up for decades. This includes restoring gut and liver health so that health-giving nutrients are better absorbed.
(b) Sleeping all night so we repair and heal.
(c) Adjusting our lifestyle to match research on women’s healthy ageing studies rather than lifestyle strategies that aren’t targeted to our changing hormones in menopause. What we have to do is to discover how to manage our lifestyle for our health as we age and if you are overweight, then look at what I have for you in the ‘Transform Me programme. If you are thinner or leaner, then discover how to turn around your symptoms using my powerful ‘Circuit Breaker’ programme.
Both programmes are changing women’s lives for the better. When you are ready I hope you will be able to join me sometime too.
Dr Wendy Sweet (PhD)/ Women’s Healthy Ageing Researcher/ MyMT™ Founder & Coach.
References:
Arigo D, Romano KA, Pasko K, Travers L, Ainsworth MC, Jackson DA, Brown MM. A scoping review of behavior change techniques used to promote physical activity among women in midlife. Front Psychol. 2022 Sep 21;13:855749.
Cadegiani FA, Kater CE. Hormonal aspects of overtraining syndrome: a systematic review. BMC Sports Sci Med Rehabil. 2017 Aug 2;9:14.
Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015 Nov;8(3):143-52.
Jaqua E, Biddy E, Moore C, Browne G. The Impact of the Six Pillars of Lifestyle Medicine on Brain Health. Cureus. 2023 Feb 3;15(2):e34605.
LaRocca TJ, Martens CR, Seals DR. Nutrition and other lifestyle influences on arterial aging. Ageing Res Rev. 2017 Oct;39:106-119. doi: 10.1016/j.arr.2016.09.002.
Mair KM, Gaw R, MacLean MR. Obesity, estrogens and adipose tissue dysfunction – implications for pulmonary arterial hypertension. Pulm Circ. 2020 Sep 18;10(3):2045894020952019.
Mohd Azmi NAS, Juliana N, Azmani S, Mohd Effendy N, Abu IF, Mohd Fahmi Teng NI, Das S. Cortisol on Circadian Rhythm and Its Effect on Cardiovascular System. Int J Environ Res Public Health. 2021 Jan 14;18(2):676.
Plunk EC, Richards SM. Epigenetic Modifications due to Environment, Ageing, Nutrition, and Endocrine Disrupting Chemicals and Their Effects on the Endocrine System. Int J Endocrinol. 2020 Jul 21;2020:9251980.
Saji Parel N, Krishna PV, Gupta A, Uthayaseelan K, Uthayaseelan K, Kadari M, Subhan M, Kasire SP. Depression and Vitamin D: A Peculiar Relationship. Cureus. 2022 Apr 21;14(4):e24363.
Siddiqui R, Makhlouf Z, Alharbi AM, Alfahemi H, Khan NA. The Gut Microbiome and Female Health. Biology (Basel). 2022 Nov 21;11(11):1683.
Silva TR, Oppermann K, Reis FM, Spritzer PM. Nutrition in Menopausal Women: A Narrative Review. Nutrients. 2021 Jun 23;13(7):2149.
Sultan S, Taimuri U, Basnan SA, Ai-Orabi WK, Awadallah A, Almowald F, Hazazi A. Low Vitamin D and Its Association with Cognitive Impairment and Dementia. J Aging Res. 2020 Apr 30;2020:6097820.

