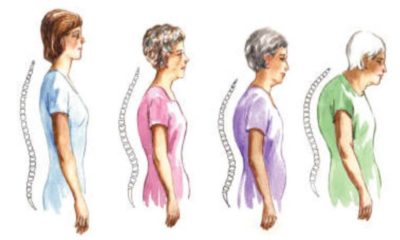
Have you ever thought about your skeleton as a metabolically active organ? I know that I never really thought about this when I went into peri-menopause and thought that the activity that I was doing, e.g. some cardio, my once a week BodyPump class and doing some exercise on most days of the week was enough to help strengthen my bones. But what I hadn’t factored in was menopause. It’s the time of our life-cycle that we not only can experience a loss of bone minerals, but we can also have some disruption to the integrity of the bone matrix or structure and this can lead to both osteopenia and then onto osteoporosis. We know a lot more about these conditions thanks to all the research that has been conducted on our mother’s generation i.e. older women, that it makes sense to remind ourselves that this is our risk too and the earlier we think about bone disease, the better we are to reduce our risk! So, let’s talk about bones and the powerful effect menopause has on their integrity and strength.
 Our beautiful bones continue to remodel throughout our life. What that means is that our bone cells break down and new bone cells are formed. It’s quite scary to think that about 1/3 of adult bone mineral is deposited in our bones during adolescence and starts to decline from our 30’s onwards. But we can’t turn back time if we weren’t active and eating well back then, so the key issue for all of us to remember, is that bone turn-over and bone re-modelling are tightly regulated through a powerful combination of hormones, minerals (nutrition), genetics and our lifestyle, so the good news is that we can do something about preventing worsening decline in this risky stage of our life. And even if you are just beginning your peri-menopause transition and are in your late-40’s, then there is no better time to think about bone health than now, whilst the rest of us already in post-menopause, have to play ‘catch-up’! So, this is a shout-out for strong women, strengthening their bones!
Our beautiful bones continue to remodel throughout our life. What that means is that our bone cells break down and new bone cells are formed. It’s quite scary to think that about 1/3 of adult bone mineral is deposited in our bones during adolescence and starts to decline from our 30’s onwards. But we can’t turn back time if we weren’t active and eating well back then, so the key issue for all of us to remember, is that bone turn-over and bone re-modelling are tightly regulated through a powerful combination of hormones, minerals (nutrition), genetics and our lifestyle, so the good news is that we can do something about preventing worsening decline in this risky stage of our life. And even if you are just beginning your peri-menopause transition and are in your late-40’s, then there is no better time to think about bone health than now, whilst the rest of us already in post-menopause, have to play ‘catch-up’! So, this is a shout-out for strong women, strengthening their bones!
One of these women is the amazing Sue Coleman-Price.
 I first met Sue when I taught her to be a Certified Personal Trainer at AUT in Auckland. I was so impressed with her work with clients from all walks of life who live in Kaikohe, Kerikeri and Whangarei, all towns of the north in the top of the North Island in New Zealand, that I have followed her progress for years. Next week we are teaming up to do some seminars up in that part of New Zealand – I can’t wait! In 2009, she won the Personal Trainer of the Year Award from Fitness NZ (now the Exercise Association of NZ) and I was thrilled with the commitment and dedication she puts into her job. Not only for clients, but as a community member and as an athletics coach for high-school athletes. She is one busy lady and like me, is passionate about women understanding how to manage themselves in their menopause transition and beyond.
I first met Sue when I taught her to be a Certified Personal Trainer at AUT in Auckland. I was so impressed with her work with clients from all walks of life who live in Kaikohe, Kerikeri and Whangarei, all towns of the north in the top of the North Island in New Zealand, that I have followed her progress for years. Next week we are teaming up to do some seminars up in that part of New Zealand – I can’t wait! In 2009, she won the Personal Trainer of the Year Award from Fitness NZ (now the Exercise Association of NZ) and I was thrilled with the commitment and dedication she puts into her job. Not only for clients, but as a community member and as an athletics coach for high-school athletes. She is one busy lady and like me, is passionate about women understanding how to manage themselves in their menopause transition and beyond.
For decades we’ve been told that osteoporosis is just one of the diseases that women might experience as they get into older-age (over 65 years). In New Zealand, it is well recognised by the Ministry of Health as a disease that most often affects post-menopausal women – and yes girls’, you can be too thin! But I think that waiting until you are through menopause and out into post-menopause (when your periods have ceased for a year or more) may well be too late. Which is why I was heartened to read in the 2016 Review of Osteoporosis from Marlena Kruger and Frances Wolber*, that as we get to menopause, disruption to bone strength and density can speed up and this happens from the age of around 50 years and it affects women from all ethnicities, not just Caucasian [European] women. The authors also highlighted that it’s not just osteoporosis that we should be concerned about, but another condition called osteopenia.
Osteopenia needs to be on our radar too. It’s a condition that occurs when there is an imbalance between bone resorption of minerals and bone formation. Essentially, it’s the early stage of osteoporosis but doesn’t necessarily progress to full osteoporosis. There is great information on the Osteoporosis website in New Zealand and where-ever you live in the world, check out your local osteoporosis guidelines for your country as well. They are full of important information to have in your menopause-toolbox too.
But it’s not just about osteopenia and osteoporosis – the clinical names given to changes to our bones making them more brittle. There is another condition which hits us in menopause due to our changing reproductive hormones. This condition is the muscle-loss condition called SARCOPENIA.
 Have some of you noticed that you are losing muscle mass as you transition through menopause and the muscle is replaced with fat? Yes, me too! All of those healthy, strong muscles that I worked hard on building up for years, suddenly seemed to disappear overnight. Eek! This is because, in menopausal women, low levels of oestrogen and changing testosterone levels too, cause muscles to lose volume and size. But here’s the thing, body fat does not protect against osteoporosis development either.
Have some of you noticed that you are losing muscle mass as you transition through menopause and the muscle is replaced with fat? Yes, me too! All of those healthy, strong muscles that I worked hard on building up for years, suddenly seemed to disappear overnight. Eek! This is because, in menopausal women, low levels of oestrogen and changing testosterone levels too, cause muscles to lose volume and size. But here’s the thing, body fat does not protect against osteoporosis development either.
This is why strengthening our muscles is just as important for us as strengthening our bones. Because if our muscle density is reducing and our fat levels are increasing, not only do we become weaker, but there is less stress being placed on your bones from the movement of MUSCLE, TENDONS and LIGAMENTS pulling on the ends of your bones. Pulling and pushing actions affect bone cell turn-over too. The ends of your bones (the epiphysis) are where you get NEW BONE CELLS forming and the epiphysis responds to pushing and pulling activities. These activites help to re-model the bone which then requires critical bone-building nutrients, such as Vitamin D, calcium, magnesium and phosphorous, to help healthy, new bone cells to be formed. But here’s the thing – hormonal changes in MENOPAUSE, and other factors such as gut inflammation can INHIBIT the uptake of these vital nutrients into our bones. But there are OTHER FACTORS impacting on bone disease risk too. These include:
1. Decreased physical activity as you age, especially some IMPACT and STRENGTH activity.
2. Decreased amino-acid (protein) intake and uptake due to changing LIVER inflammation. Proteins are ‘turned-over’ in your liver and if you aren’t getting adequate healthy proteins into your diet, then this can have a down-stream effect on sarcopenia too.
3. Loss of activation of the motor-units (nerves) which stimulate muscles to contract. Muscle movement is controlled by your nervous and hormonal system and when we activate all of our muscles, then this is great for bone and muscle strength. It’s where the old term ‘use it, or lose it’ comes from. When your muscles are stimulated to pull on bones, then your bones are also stimulated to turn-over new bone cells.
4. Age-related decline in the hormones which assist your bones to stay strong, i.e. testosterone, growth hormone, Vitamin D and IGF-1.
5. INTERNAL INFLAMMATION. For example, gut inflammation can inhibit the uptake of KEY nutrients that support bone health as does not sleeping well overnight. If you aren’t sleeping, your body isn’t healing and repairing itself.
6. The wrong DIET for menopause. A typical Western diet that is high in processed foods, sugar and alcohol is typically not osteopenia or osteoporosis friendly. This is why I say when it comes to menopause and the risk of oesteoporosis with age, we all need to improve our diet to better meet our changing hormonal environment which will become our ‘new-normal’ the older we get.
7. Being too THIN and SMALL IN STATURE. If you have a thin bone structure, and weigh UNDER 60 kg, then you are at greater risk for osteoporosis as you get older. Your goal therefore is to increase your muscle mass and maintain a body weight that decreases your risk as you age.
This is why I want to remind you about exercise – especially exercise that will help your bones and muscles as you get older. Even if we didn’t do too much exercise in our younger days (although many of us did and now we have gotten out of it), then we need to keep exercising! As the World Health Organisation Bulletin (2003) on how to de-fuse the osteoporosis time-bomb reminds us –
‘Exercise minimizes bone loss later in life. Not only does exercise improve bone health, it also increases muscle strength, coordination, balance, flexibility and leads to better overall health. Walking, aerobic exercise, and t’ai chi are the best forms of exercise to stimulate bone formation and strengthen the muscles that help support bones. Encouraging physical activity at all ages is therefore a top priority to prevent osteoporosis.’
[Chan, K., Anderson M., & Lau, E. (2003). Exercise interventions: defusing the world’s oesteoporosis time bomb. WHO Bulletin]
Do you know what your RISK for osteoporosis is? If you don’t, then go and get your bone density tested. If you are concerned about your changing bone strength and density, then make sure you talk to your health or medical professional so you can get this tested. Clinically the ‘gold-standard’ for measuring bone density is a Dual Energy X-Ray Absorptiometry or DEXA scan and is available through your health provider.
But whether you are at risk or not, then I also encourage you to visit the website and look at the MyMT™ Re-Build My Fitness programme. Waiting for you here are gentle to intermediate exercise programmes (including pre-activity screening processes that allow you to decide if you are ready for exercise or you need medical permission), which progress you into exercise that is suitable for you as a woman going through menopause. These are not advanced programmes because those of you who are highly experienced, typically are also highly motivated! But I am so passionate about getting women back into healthy exercise as they age, that I have designed this programme with this purpose in mind. The programmes can be down-loaded and I have webinars and videos to explain the exercises to you. Even if you go to the gym, there are programmes that suit your needs either at home or with gym-based equipment. I’ve designed everything you need for your EXERCISE NEEDS as you age. The programmes are progressive and designed for both beginners and intermediate level women to build their stamina through walking or other cardiovascular exercise, build their strength, flexibility, balance and help to stabilise the core muscles which support posture and stability. All factors which influence health and wellbeing as we age!
 Everything you need to know about how to rebuild your exercise routines and take back control of your exercise for your menopause transition is all in the 6-Step MyMT™ Re-Build Me EXERCISE modules. These exercise modules are also designed to follow-on from the 12 week MyMT lifestyle change programmes that help women to lose weight and manage their sleep and hot flushes naturally. Despite 30 years in the fitness industry and fitness education, reaching peri-menopause made me feel exhausted and sore when I did all the exercise that I had been doing for years. That’s why I tell women who are doing lots of high-intensity exercise, that until they are sleeping all night, then they need to tone-down the intensity of their workouts. I know we all have learnt to ‘push-through’ with our exercise because it has been the one thing that has helped us cope over the years, but sometimes too much exercise can send us into more exhaustion, sleep deprivation and hot flushes, because our chronic stress hormone called ‘cortisol’ stays elevated. When cortisol stays higher than it should, there is a negative impact on our menopause symptoms too, especially our sleep and energy levels.
Everything you need to know about how to rebuild your exercise routines and take back control of your exercise for your menopause transition is all in the 6-Step MyMT™ Re-Build Me EXERCISE modules. These exercise modules are also designed to follow-on from the 12 week MyMT lifestyle change programmes that help women to lose weight and manage their sleep and hot flushes naturally. Despite 30 years in the fitness industry and fitness education, reaching peri-menopause made me feel exhausted and sore when I did all the exercise that I had been doing for years. That’s why I tell women who are doing lots of high-intensity exercise, that until they are sleeping all night, then they need to tone-down the intensity of their workouts. I know we all have learnt to ‘push-through’ with our exercise because it has been the one thing that has helped us cope over the years, but sometimes too much exercise can send us into more exhaustion, sleep deprivation and hot flushes, because our chronic stress hormone called ‘cortisol’ stays elevated. When cortisol stays higher than it should, there is a negative impact on our menopause symptoms too, especially our sleep and energy levels. 
That’s why I’m targeting what to do in our menopause transition – it’s a stage of our lives that hasn’t been well promoted in exercise prescription and exercise physiology and I’m on a mission to change this! Exercise has been such a big part of my life and maybe it has for you too. Or maybe it used to be and you would like to feel motivated and educated to make it part of your life again. If so, I hope you can join me on MyMT.
- Chan, K., Anderson M., & Lau, E. (2003). Exercise interventions: defusing the world’s oesteoporosis time bomb. WHO Bulletin]
- Kruger, M. & Wolber, F. [2016]. Oesteoporosis: Modern paradigms for last centuries bones. Nutrients (8),376, 1-12.
- Lohana, C. & Samir, N. (2016). Risk Management of Osteoporosis in Postmenopausal Women. Global Journal of Health Science, Vol. 8, No. 11; 36-44

