“I have an idea for your newsletter” mentioned Lesley. “I keep waking up to muscle cramps and I have no idea why. My daughter gets them too.”

This is Lesley in the photo above. She’s a runner and recently completed the MyMT™ Transform Me programme. It’s been such a privilege to get her back into running and helping her to feel better. Her story is HERE.
Night leg cramps, also called nocturnal leg cramps, are painful, involuntary contractions or spasms of muscles in your legs, usually occurring when you’re in bed. I think most of us have felt the spasms that hit us as we are just getting off to sleep, or for me, rolling over in bed. Many a night I would get out of bed and stand on the cold bathroom floor and stretch out my hamstrings. Whilst night leg cramps usually involve your calf muscles, other muscles in your feet or thighs might cramp as well. Forcefully stretching the contracted muscle relieves the pain but the most important thing is to have a focus on the nutrients that we need as we move through menopause.
I’ve taught students about muscle cramps for years. They are a topic of interest for numerous sport and exercise science students. When I began to experience muscle cramps myself, I was quite surprised, because I certainly wasn’t doing the exercise that I used to which is often associated with muscle cramps and spasms. But as I looked into the cause of them as one of the numerous symptoms of menopause (as is restless leg syndrome), I also began to understand that low oestrogen affects how our muscles contract – and this in turn affects muscle cramps, especially at night.
Cramps occur when a muscle is not able to relax properly (such as from a deficiency of magnesium or potassium in your diet) or for those of you who are regular exercisers, the muscles can also become irritated by a buildup of lactic acid (which can happen if you don’t rest your muscles after exercising). On top of this, dehydration can worsen both of these problems.
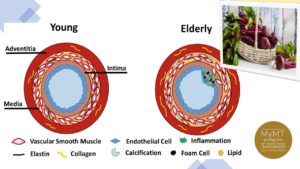
For those of you who have been following me for a while and reading my weekly newsletter, you will be familiar with my articles about our ageing blood vessels and how these change as we lose oestrogen. Our blood vessels lose some of their elasticity as we move through menopause and therefore, become ‘stiffer’. It’s known as ‘arterial stiffness’ and is a known contributor to cardiovascular disease as we get older. As such, this arterial stiffness which causes reduced blood flow to the muscles, can also cause cramps at night. The narrowing of the arteries to your legs caused by the loss of elasticity as well as increased inflammation for those of you doing a lot of physical exercise, or if you are on your feet every day, can contribute to your nocturnal cramps (and may well be contributing to your hot flushes and night sweats too).
However, there may well be other reasons for your leg cramps as well. You may also be deficient in certain nutrients in your diet, especially calcium, magnesium and of course, Vitamin D.
To mitigate the ‘perfect storm’ between our changing oestrogen levels and our changing muscles and blood vessels in menopause, and to reduce the risk of nocturnal cramping, we need to focus on a few nutrients in our diet. Magnesium is a nutrient I spoke about last week in my newsletter (CLICK HERE) and the other nutrients that matter are both calcium and Vitamin D. These nutrients will help you to prevent your nocturnal cramps (as will adequate hydration).
I often call calcium the ‘forgotten’ mineral for our muscles because so much emphasis is given to it’s opposing mineral, magnesium. As well, with post-menopause bone health a topic of interest from the perspective of the high incidence of osteoporosis as women age, calcium is an important mineral for our bone health. But there’s another reason calcium is important, and this is because calcium acts as a crucial nerve transmitter. It is needed for the regulation of muscle contraction. Because nocturnal cramps are an irregularity of the muscle contraction process, we musn’t forget about calcium.
Calcium helps the electrical nerve signal ‘jump’ from the nerve ending to the muscle. This is how muscles contract. They need calcium. I’ve been telling sport and exercise students this for decades. As I’ve put up lecture slides about how muscles contract and interact with the nervous system, I always said to students, “Don’t forget about the importance of calcium in your diet, and especially don’t forget about Vitamin D and folate. Both these nutrients help calcium to be absorbed in the small intestine and you need calcium to help your muscles contract and for your recovery.”
The reason I used to say this, is because skeletal muscle contraction needs calcium. Muscles contract when an electrical current from the nerve endings sends signals for the release of calcium from inside the part of the muscle called the sarcoplasmic reticulum.
Without adequate calcium, you are going to get muscle cramps, numbness and tingling as well as dry skin and other ailments associated with menopause and post-menopause. For those of you, like Lesley, who do a lot of exercise, then you need to ensure that both magnesium and calcium intake from food (and not supplements) is adequate every day.
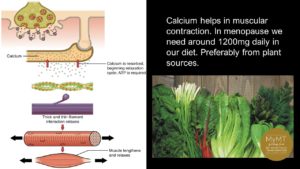
It makes sense that if we are regularly exercising, then we need calcium in our diet every day. In fact, we need 1200mg a day, day after day … because our body doesn’t make it or store it for long either. Life without adequate calcium from foods in our diet is impossible. And yes, if you are in post-menopause, you need it for your heart health as well as bone health too.
Foods that supply calcium:
Whilst dairy products contain relatively high amounts of calcium, these aren’t always tolerated in the diet, especially for those of you with food allergies or lactose intolerance or who want to lose weight. Hence, I promote lots of different foods that women can add to their diet to get adequate calcium and I have comprehensve lists in the MyMT Food Guide in all of my 12 week programmes. In many parts of the world, e.g. Okinawa, China and other Asian countries, whereby vegetarianism is a way of life, women meet their daily calcium needs, not by drinking milk, but by eating other types of foods. Three of these foods are:
- Tofu: 100 grams of tofu has about 120mg of calcium
- Spinach: 1 cup of cooked spinach has approx. 244mg of calcium.
- White beans: 1 cup of cooked white beans has approx. 160mg of calcium.

Calcium as a nutrient is most ,commonly associated with the formation
and metabolism of bone but it is also an important mineral in muscle contraction and this includes both the skeletal and cardiac muscles. Calcium in the circulatory system, extracellular fluid, muscles, and other tissues is also critical for mediating blood vessel contraction and dilatation as well as enhancing nerve transmission. It’s an important mineral.
When we don’t get enough calcium in our diet, then calcium is ‘stolen’ from bone tissue, which serves as a reservoir for and source of calcium for these critical metabolic needs. Furthermore, calcium metabolism is regulated by the parathyroid hormone (PTH)–vitamin D hormonal system, so managing and checking Vitamin D status as you move through menopause is important for you to remember as well.
When our symptoms over-whelm us in menopause, it’s difficult to ascertain why. But as I always say to women who join me on the online 12 week MyMT™ programmes, “it’s important to understand that our body is changing and lowering oestrogen and progesterone are a normal part of menopause. What we need to know, is how to look after ourselves in a changing hormonal environment, that is the gateway to our biological ageing.”
References:
Kuo, I. Y., & Ehrlich, B. E. (2015). Signaling in muscle contraction. Cold Spring Harbor perspectives in biology, 7(2), a006023. https://doi.org/10.1101/cshperspect.a006023
Institute of Medicine, ( 2011). Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press
Szent-Györgyi A. G. (1975). Calcium regulation of muscle contraction. Biophysical journal, 15(7), 707–723. https://doi.org/10.1016/S0006-3495(75)85849-8

