If you cast your mind back to your transition through puberty, I wonder if at times, you felt moody, melancholy, grumpy, or angry? Perhaps you felt worthless or un-motivated at times. Perhaps you feel that you’ve lost any propensity for experiencing pleasure in your life from normally pleasurable life events – a description of Anhedonia – a word I didn’t even know existed, until I was researching menopause and my emotional state.
Perhaps you used to feel angry or easily irritated during puberty? Perhaps you were a ‘door-slammer’ (as I was) – goodness knows how my mother coped with this in an old, rural house where the slamming of a door reverberated throughout!
Back in those days, I didn’t know that my changing hormones were to blame. Over 45 years ago, I don’t think any of us even gave our pubescent hormonal changes a thought, including that these hormonal changes could be linked to our moods and melancholy, did we?
But here we are, arriving in our menopause transition and perhaps, as happens for millions of women world-wide, you feel a bit floored.
Perhaps memories of the emotional upheaval of your mental health in puberty come to the fore. But if all these mental health changes are arriving back during our menopause transition, what’s going on? Why is this? And why, as I used to think to myself, am I being offered anti-depressants as the first line of treatment, when I’ve been happy and healthy for years?
When I learnt from my academic studies, that 1 in 5 New Zealand women get placed on anti-depressants in their mid-life menopause transition and 2/3 of women in the United Kingdom, Australia and New Zealand who are placed on anti-depressants are female and typically in their 50s and 60s, I was quite surprised.
But that was before peri-menopause mood swings and melancholy found their way to me as well.
I was 51 years old and I remember vividly, the day I left my high-intensity spin class at the gym and after walking out to my car, felt like bursting into tears. Where all those exercise-fueled endorphins went at the time is beyond me!
The link between depression and menopause has been known for years.
This is why for so many women, anti-depressants during menopause are an important intervention and if you are feeling down and out, then always seek support from your medical specialist as well.
Whilst I visited my own GP about my moods and feeling low, but before deciding to go on medication, I wanted to understand the link between depression and menopause more thoroughly. I was curious to understand why I had been so happy, motivated and healthy all my life, but hitting peri-menopause sent my moods and feelings of worthlessness into a tail-spin. As such, I spent hours researching how depression manifests in menopause (not clinical depression that is diagnosed differently in younger people).
So, if you are feeling out of sorts and well … down in the dumps with little or no motivation, then here’s what I want to share with you:
- Depression is linked to the build-up of inflammation. As we age, our body becomes more inflamed – a natural part of our biological gateway into ageing. Inflammation is exacerbated with our changing temperature regulation too as our body struggles to cool down due to the role that declining oestrogen plays on our vascular system – our blood vessels become ‘stiffer’.
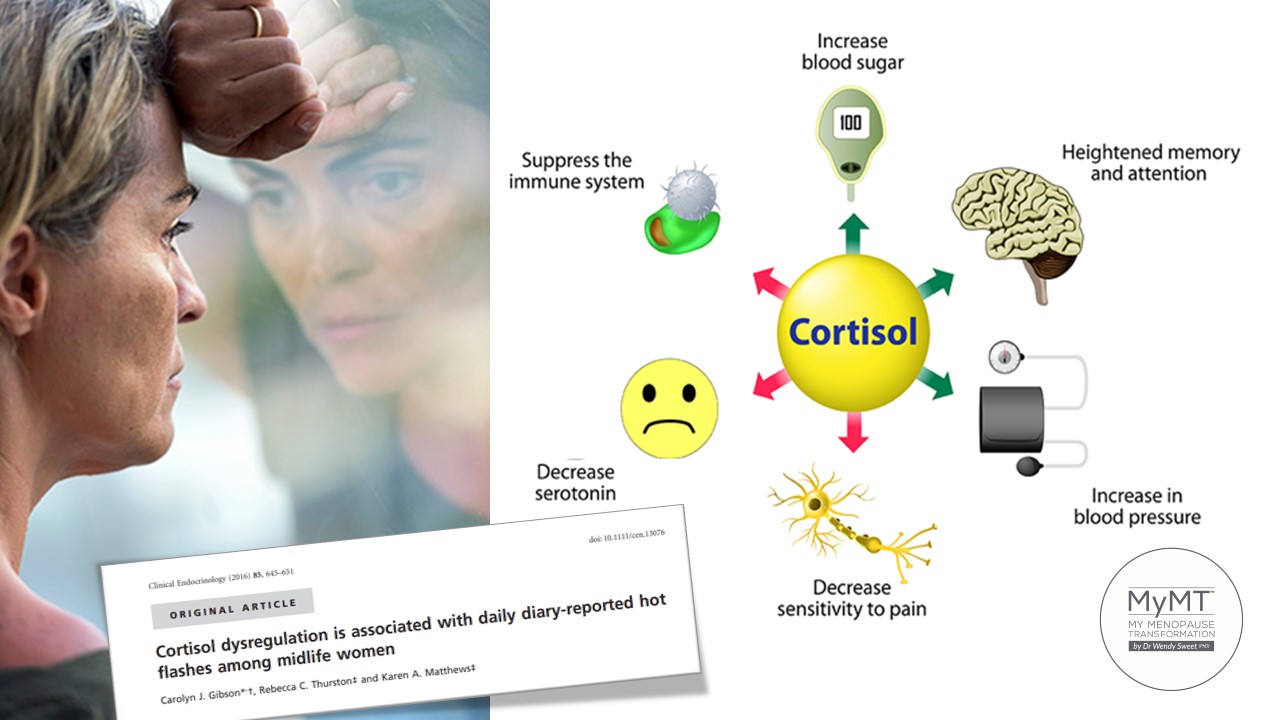
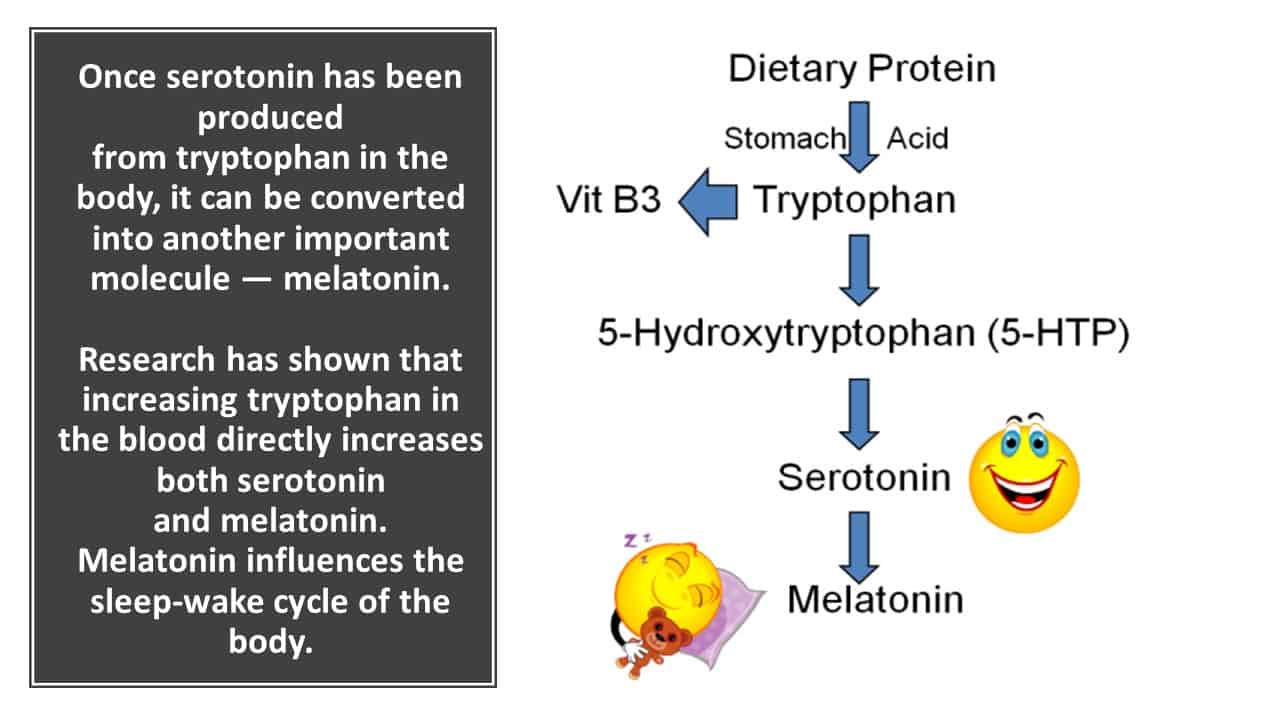
When Hot Flushes are more than 5 an hour, our body overheats and becomes inflamed. This inflammation then exacerbates a decrease in SEROTONIN. This important hormone is your ‘happy hormone’. When oestrogen is lowering in menopause, serotonin follows it on a downward slide. But there’s another factor as well.
If you aren’t sleeping and you are feeling stressed, then you may be producing too much of your chronic hormone, Cortisol. This causes more inflammation in your organs, muscles and blood vessels as we biologically age. The accumulation of high levels of cortisol, can disrupt serotonin production more rapidly during menopause.
- There is a very strong association between sleep disturbance and major depression (Nutt et al, 2008). For women in their menopause transition, this is tough. We all know that sleep is the nemesis of the midlife woman but sleeping less than 6 or 7 hours a night, is positively associated with worsening depression. When we aren’t sleeping during menopause, we build up oxidative stress in our heart, muscles, arteries and gut. This is why in both of the MyMT™ symptom reduction programmes, I teach women how to re-balance their sleep hormones using lifestyle strategies and of course, the circadian rhythm research specific to their menopause transition.

- Low Vitamin D3, depression and worsening inflammation go hand-in-hand. Vitamin D is often low in menopausal women because it decreases with changes to oestrogen receptors in our skin. (Lerchbaum, 2013). I talk a lot about Vitamin D and this connection with menopause with women, because so many of us work inside and if women have darker skin, then their Vitamin D absorption is lower too. If women are also overweight and carrying more belly fat, then because Vitamin D has an affinity to fat in fat storage areas, then the Vitamin D can go to adipose tissue and not to where it is needed – in muscles, bones, nerves and the heart. [Dregan, Rayner, et al., 2020). Whilst it doesn’t matter if you are going on Menopause HRT or other medications such as anti-depressants, please ask your Doctor to also check your Vitamin D levels, especially those of you who are emerging from a Northern winter.
- Is your intake of B vitamins low and how is your liver health? When Liver inflammation is present in cells and tissues (known as Non-Alcoholic Fatty Liver Disease or NAFLD) or if women are putting on belly fat and have poor gut health, then B vitamins are not absorbed and metabolised very well. Low Vitamin B6 and B12 increases depressive episodes (Feraj, 2017). This is why, for women who want to improve their moods and motivation during menopause, it’s important to turn around liver health first, especially for women who are overweight.
Changing gut health and factors such as PCOS (Polycyctic Ovarian Syndrome) as well as insulin resistance (pre-diabetes) and peri-menopuase changes are also implicated in NAFLD development. (Carrieri, Osella et al, 2022).

- The gut-brain connection has become an important factor in menopause depression research. Changes to our food production and processing as well as menopause hormonal changes impacts our gut health during midlife. Numerous women develop Irritable Bowel Syndrome (IBS) or Diverticulitis when they reach their 50’s. With researchers now understanding the powerful connection between our immune system and our gut, this has a profound effect on our mental health if our gut health is impaired.
This is to do with the accumulation of gut inflammation, which may impact on the absorption of a protein called Tryptophan. This important protein is needed in the pathway to make your mood-hormone, serotonin. Tryptophan is absorbed into the capillaries in the intestinal wall. A small amount of the amino acid remains free while the majority of it (roughly 80%–90%) is transported bound to albumin through the blood and into the brain, and it is converted into melatonin via the serotonin pathway. (Laudisio, Barrea et al, 2020).
The great news from so many of the studies that became part of my menopause symptom reduction research, was that many of these came to a similar conclusion to the research by Taylor and Hickey (2014):
Lifestyle factors, such as managing BMI (Body Mass Index) and improving sleep could be used together with nutritional interventions to aid in efforts to prevent or help treat depression in women during the menopause transition.
Feeling depressed or experiencing frequent mood swings in peri-menopause and menopause is all about the connection between all of your hormones – not just oestrogen, progesterone and serotonin. Obviously, talk to your Doctor about how you are feeling, but also focus on your diet, sleep, exercise and stress management.
I’m always reminding women that our body does not work in isolation. All of our organs in the body are connected via chemical messengers, called hormones. They work synergistically together. The role they play inside your body is to maintain the body in ‘homeostasis’.
This is a term that physiologists and endocrinologists refer to as ‘maintaining the body in a state of equilibrium’. So when one hormone is low, there are chemical and neurological messages sent to other hormones to counteract the environment changes that the low hormone is causing.
As women transition from peri-menopause to menopause, the production of oestrogen is declining. Because oestrogen is a hormone, when levels are lowered it affects the function of not only progesterone, but other hormones in the body as well, including your mood hormone, serotonin. When serotonin levels are low, this impacts on other hormones produced by your thyroid, adrenal and more importantly, your pituitary glands where serotonin production occurs.
Are there lifestyle solutions to help my moods and motivation during menopause?
Absolutely YES! If you are experiencing mild to moderate depression or frequent mood swings in menopause, then you can reverse this. You need to follow a specific regime for sleeping, eating, moving and boosting Vitamin D production as well as reducing any inflammation and managing menopause weight gain.
You also need to focus on any gut and liver health repair and your nutrition and sleep, before launching into any vigorous exercise programmes. When you aren’t sleeping, then too much exercise can worsen hot flushes, moods and send you into adrenal fatigue which of course crashes your energy levels too.
Brining all this together for you in one progressively-delivered lifestyle programme is what My Menopause Transformation is all about. And in my private coaching community that sits alongside your private member area, I’m with you every step of the way.

References:
Boulkrane MS, Fedotova J, Kolodyaznaya V, Micale V, Drago F, van den Tol AJM, Baranenko D. Vitamin D and Depression in Women: A Mini-review. Curr Neuropharmacol. 2020;18(4):288-300.
BMJ 2014; 349 doi: https://doi.org/10.1136/bmj.g7641. One in 10 women in England takes antidepressants, survey shows (Published 15 December 2014) BMJ 2014;349:g7641
Carrieri, L., Osella, A.R., Ciccacci, F.; Giannelli, G.; Scavo, M.P. (2022). Premenopausal Syndrome and NAFLD: A New Approach Based on Gender Medicine. Biomedicines, 10, 1184.
Dregan, A., Rayner, L., Davis, K., Bakolis, I., Arias de la Torre, J., Das-Munshi, J., Hatch, S. L., Stewart, R., & Hotopf, M. (2020). Associations Between Depression, Arterial Stiffness, and Metabolic Syndrome Among Adults in the UK Biobank Population Study: A Mediation Analysis. JAMA psychiatry, 77(6), 1–9. Advance online publication. https://doi.org/10.1001/jamapsychiatry.2019.4712
Feraj, J. (2017). Micro-nutrients, depression and inflammation among women of reproductive age. Doctoral Dissertation 993, University of Massachusetts.
Gibson CJ, Thurston RC, Matthews KA. (2016). Cortisol dysregulation is associated with daily diary-reported hot flashes among midlife women. Clin Endocrinol (Oxf). 85(4):645-51. doi: 10.1111/cen.13076.
Laudisio D., Barrea L., Pugliese G., Aprano S., Castellucci B., Savastano S., Colao A., & Muscogiuri G. (2020). A practical nutritional guide for the management of sleep disturbances in menopause. Int J Food Sci Nutr. 72(4):432-446.
Lerchbaum, E. (2014). Vitamin D and menopause – A narrative review. Maturitas Journal, 79, 3-7
Ministry of Health Public Health Report 43 (2007). Patterns of Antidepressant Drug Prescribing and Intentional Self-harm Outcomes in New Zealand: An ecological study.
Nutt, D., Wilson, S., & Paterson, L. (2008). Sleep disorders as core symptoms of depression. Dialogues in clinical neuroscience, 10(3), 329–336. https://doi.org/10.31887/DCNS.2008.10.3/dnutt
Vivian-Taylor & Hickey, M. (2014). Menopause and depression: Is there a link? Maturitas Journal, 79, 142-146
Vázquez H, Molina-López J, Herrera-Quintana L, Gamarra-Morales Y, López-González B, Planells E. Association between Body Fatness and Vitamin D3 Status in a Postmenopausal Population. Nutrients. 2020 Feb 29;12(3):667.

