What do you think about when you are lying awake at 2am, or 3am or 4am?
Do you plan your day ahead or are you just despairing because night after night you aren’t sleeping and you can feel your energy being sucked out of you?
You know that the day ahead is another busy one and your brain will be fuzzy and fatigued. You won’t be functioning at your best will you?
If you feel like this, then you aren’t alone. I was like that too, so please keep reading.
What you may not realise is that wakefulness, light sleeping and insomnia (not being able to get back to sleep), isn’t just linked to your changing reproductive hormones during menopause, but to a number of other factors too.
For women in their menopause and post-menopause years, these factors include:
- low Vitamin D,
- low iron,
- low calcium intake,
- too much protein and,
- the stressful life of the modern, busy woman.
But perhaps of more concern, is that the longer you lie awake night after night, the more your hot flushes and/or weight gain and immune health may become worse over time too.
For many women, as I found myself, the HRT kicks in for a while, but not changing our lifestyle to allow our body to adapt to midlife hormonal changes, then sleep problems can stay around.
Why your Sleep is important to conquer during or beyond Menopause
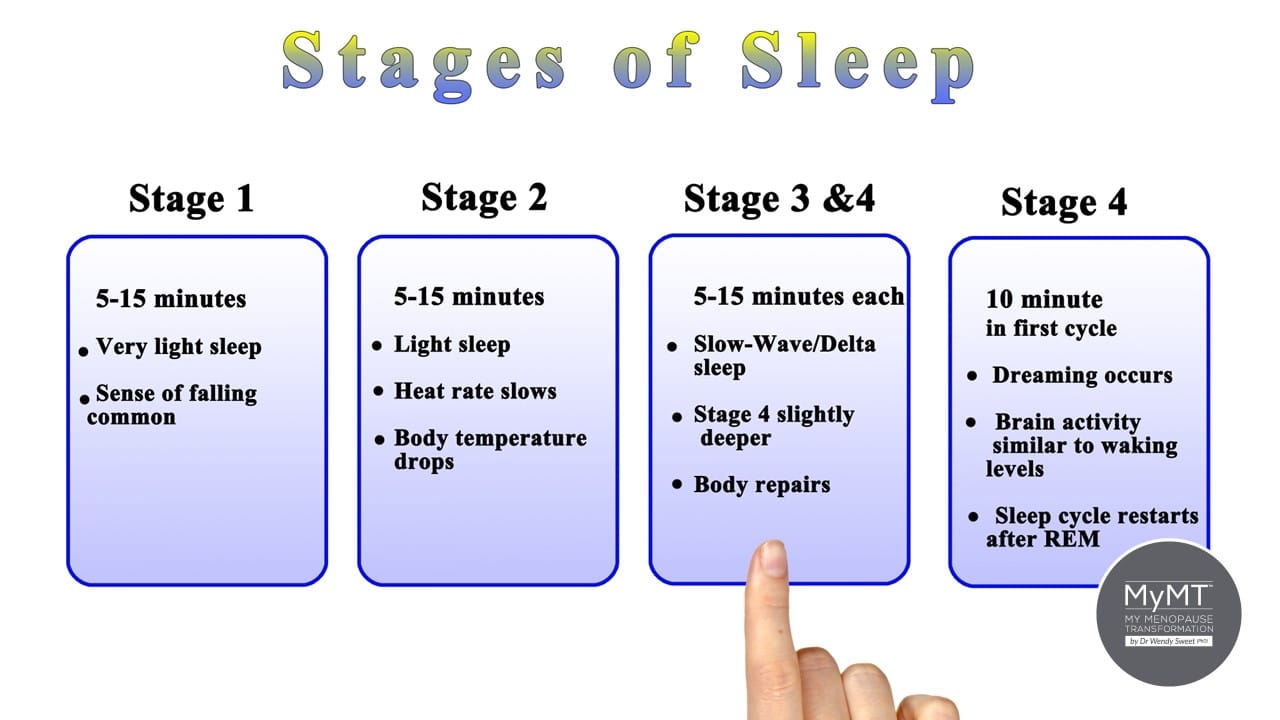
Scientists divide sleep into two major types: REM (rapid eye movement) sleep or dreaming sleep, and non-REM or quiet, healing sleep. Sleep specialists have called non-REM sleep “an idling brain in a movable body.”
During this phase, thinking and most bodily functions slow down, but movement can still occur, and a person often shifts position while sinking into deeper stages of sleep.
When we go to bed and start to fall asleep, both phases last around 4 hours or more.
Your deep sleep lowers your blood pressure - this is important to reduce night sweats.
After your REM sleep, comes your deeper sleep, or your non-REM sleep. This is characterised by slow brain waves called delta waves. When your brain slows down, your body enters deep sleep.
Breathing becomes more regular and it’s an important stage for your blood pressure to fall. The pulse slows to about 20% to 30% below the waking rate.
This stage is also when your brain is less responsive to external stimuli, making it difficult to wake up. But if your blood pressure doesn’t fall, then many women may wake up to hot flashes/flushes or night sweats at this time of night – even those of you in your post-menopause years.
That’s why, in my sleep module in the MyMT™ programs, I have a focus on how to reduce your blood pressure before bedtime, so you are entering your deep sleep with a lowered blood pressure.
When you do this, you fall into a deeper, restorative sleep more quickly. It’s this deep sleep that is really important for us to have during and after menopause, because this is the time that your body heals, and cells and tissues both repair and renew, especially your muscle tissue.
But there’s more to the sleep story during menopause. We need to have deep sleep in order to activate our immune system and reduce fatigue.
Understanding this, is crucial for those of you who are doing heavy exercise. You have to be sleeping well for your muscles to recover.
Reduce your Fatigue and Improve your Immune Health
Menopause insomnia not only causes your performance to drop, but your muscles and joints may remain sore for longer, hence, you don’t recover sufficiently before the next training session.
Just as deep sleep restores your body, scientists also know that REM or dreaming sleep restores your mind, perhaps in part by helping clear out irrelevant information. A very important task for a generation of women with a lot going on in their lives still!
When we get this deep, restorative sleep (between 2-4am), blood flow is directed less toward your brain, which cools measurably. At the beginning of this stage, the pituitary gland releases a pulse of growth hormone that stimulates tissue growth and muscle repair.
But if we are lying awake between 2 and 4am, then this release of growth hormone does not reach the threshold it needs to for healing and repairing our body.
As I mentioned above, this is why I hear from so many women who are avid exercisers and they don’t understand that their sore muscles and joints are due to not just low oestrogen, but also not sleeping!

Why you can't lose weight if you aren't sleeping ... neither can you build and repair muscle.
A full night’s sleep helps you to build and retain muscle. It is also necessary for weight management too.
If you aren’t sleeping well, then one of the hormones that helps with muscle recovery and repair, called Growth Hormone remains low overnight. But the blood sugar regulation hormone called insulin remains high. So too, does the chronic stress hormone called cortisol.
This powerful combination of high insulin and high cortisol competes with your sleep hormone, called melatonin. It can remain low in the evening, when it should be high, to activate your sleep drive.
Don’t forget, that as a woman transitioning menopause, your melatonin levels are already affected by your changing reproductive hormones, especially oestrogen, due to your natural ageing.
The lower that melatonin is before you go to bed and the lower it stays overnight, the more awake you feel.
The more awake you feel, the busier your brain and the more hot flushes you have …. night after night, it happens … and over time, your brain and your hormones are now reading this as your ‘new normal’.
As many of you already know – the result is daily fatigue, exhaustion, irritability and with your insulin levels all mixed up overnight, the weight starts to increase around your belly too.
That’s why in the MyMT ‘Transform Me’ weight loss programme and the MyMT Circuit Breaker symptom-reduction programme, the first module you listen to is simply called ‘Sleep All Night’.
Without this precious sleep, your body doesn’t burn fat.

The Role of Your Circadian Rhythm during Menopause and Post-Menopause is Important
In mammals, including humans, the body temperature displays a circadian rhythm.
It is maintained within a narrow range to facilitate the optimal functioning of physiological processes. Normally, your body temperature increases during the daytime and decreases during the night. [Coiffard, 2021].
Many factors may therefore, affect your body temperature, including your environment, ageing, an imbalance of hormones (especially thyroid and adrenal hormones), sickness and/or medical treatments.
Any disruption to your body temperature also affects your immune system. This is why there is a bi-directional relationship between your body temperature and your biological, circadian clock.
It’s also why, during menopause, to beat the heat, you have to sleep!
One of the strategies that women on my programmes discover is the importance of our evolutionary physiology and the role of the Circadian Rhythm on menopause insomnia.
I teach women how to adjust their circadian rhythm to specifically match their changing hormonal levels during menopause, and to help with temperature regulation, blood pressure and weight gain.

Understanding your Circadian Rhythm during and after Menopause
The term ‘Circadian’ means “about a day”. This means that your circadian rhythms are daily fluctuations in your biology. During and after menopause, these daily rhythms can become unbalanced, as declining reproductive hormones affect your sleep hormones.
When your circadian rhythm is out of balance, insomnia can follow you into your post-menopause years. For millions of women, this contributes to higher blood pressure, poor immune health and weight gain.
This internal clock, which gradually becomes established during the first months of life, controls the daily ups and downs of biological patterns, including body temperature, blood pressure, and the release of hormones.
Circadian rhythms make people’s desire for sleep strongest between midnight and dawn, and to a lesser extent in mid-afternoon.
But the changing menopause hormones may cause disruption to normal circadian rhythms, so as women transition into or through menopause, then it’s really important to restore this biological rhythm and make adjustments to get back to sleeping all night.
If women don’t achieve this, then, over time, their brain and body start to read this 2-4am ‘awake’ period as ‘normal’. Weight goes on and blood pressure starts to increase.
But here’s the thing – because hormones in the body all work in harmony with each other, when your reproductive hormones change as you go into menopause, your other hormones start to adjust to re-balance the body. Especially hormones that control your blood pressure, heat regulation, stress levels and moods.
When I began to look into our menopause symptoms as part of my women’s healthy ageing studies, I began to understand that our menopause transition is a natural transition that all women go through.
But for millions of women, this stage of their life can result in all sorts of mayhem, and it all starts with not sleeping well.

Thousands of women are experiencing the excitement and renewed energy from sleeping all night and getting rid of their hot flushes and night sweats, whether or not they are on hormonal medications.
And if you need to lose weight, then you must get your sleep sorted.
Menopause is the transition into the next phase of our lives – our ageing. As oestrogen levels naturally decline, there are numerous changes that occur in our body, from our pituitary hormones which control sleep, to our muscles to our blood sugar regulation.
I’ve pulled all the scientifically-evidenced solutions together in one fabulous programme which not only helped me, but is now ‘life-changing’ for other women too.
If you would like to join me on either of my 12 week online programmes then come on board when you can. If you are thinner you might like to look at the ‘Circuit-Breaker’ programme and if you are overweight, then look at the ‘Transform Me’ programme.
You can also start with my 2 hr Masterclass on Menopause which is updated and revised and is now in 2 parts. I have a brief video for you below as I explain why you need to watch it!
I would love you to discover how to sleep all night, reduce your symptoms in menopause and get back to feeling like the ‘old-you’ again.
Dr Wendy Sweet (PhD)/ MyMT™ Founder & Member: Australasian Society of Lifestyle Medicine
References:
D’Antono B, Bouchard V. Impaired sleep quality is associated with concurrent elevations in inflammatory markers: are post-menopausal women at greater risk? Biol Sex Differ. 2019 Jul 8;10(1):34. doi: 10.1186/s13293-019-0250-x.
Davis, S., Castelo-Branco, C. et.al. (2012). Understanding weight gain at menopause. Climacteric, 15: 419–429.
Geddes, L. (2019). Chasing the Sun: The new science of sunlight and how it shapes our bodies and minds. London: Profile Books.
Hartmann C, Kempf A. Mitochondrial control of sleep. Curr Opin Neurobiol. 2023 Aug;81:102733. doi: 10.1016/j.conb.2023.102733. Epub 2023 Jun 28. PMID: 37390796.
Harvard Health Report (2017). Improving Sleep. Harvard Health Publication
Jehan S, Masters-Isarilov A, Salifu I, Zizi F, Jean-Louis G, Pandi-Perumal SR, Gupta R, Brzezinski A, McFarlane SI. Sleep Disorders in Postmenopausal Women. J Sleep Disord Ther. 2015 Aug;4(5):212. Epub 2015 Aug 25. PMID: 26512337; PMCID: PMC4621258.
Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006 Nov 15;164(10):947-54.
Reinke H. & Asher G. (2017). Circadian clock control of liver metabolic functions. Gastroenterology, 150: 574–580.
Rizzi, M. et al. (2016). Sleep Disorders in Fibromyalgia Syndrome. Journal of Pain Relief, 5:2, 1-5
Sharma, S. & Kavuru, M. (2010). Sleep and Metabolism: An Overview. Int. Journal of Endocrinology, Article ID 270832, 1-12.
Woods, N. et al. (2009). Cortisol Levels during the Menopausal Transition and Early Postmenopause: Observations from the Seattle Midlife Women’s Health Study. Menopause, 16(4): 708–718.
Menopause and Waking at 4am, 3am and 2pm FAQ's
Waking at 4am during menopause, 3am or 2am, may be linked to hormonal changes, especially when heart rate, blood pressure and temperature don’t drop as they should during deep sleep. This disruption can trigger night sweats or hot flushes that cause early waking. The blog explains that this is often tied to the body’s struggle to move into restorative non-REM sleep, where blood pressure normally lowers and the body heals. Discover why this occurs during menopause when your hormones are declining.
When sleep is disrupted night after night, —especially between 2am and 4am— your immune system, liver and muscles are missing out on the important healing phase, which occurs overnight. During these hours, growth hormone is released to repair tissues, reduce inflammation, and support the immune system. Without this deep sleep, fatigue, muscle soreness, and slower recovery from exercise are more likely, as is worsening hot flushes, joint pain and weight gain.
One approach is to reduce blood pressure before bed to help the body enter deeper non-REM sleep more quickly. Restorative sleep is important for managing fatigue, supporting the immune system, and regulating other hormones which help to control weight changes during menopause. These hormones include insulin and cortisol – both of which may get out of balance with insomnia. Lifestyle changes are crucial to reduce night-time wakefulness.


