It was her comment in her book that piqued my interest.
“For women with mildly raised cholesterol and a lower risk of cardiovascular disease, red yeast rice preparation may offer a solution” mentioned world renowned cardiologist, Dr Angela Maas.
“Red yeast rice contains monocolin K, which is identical to the statin, lovastatin … however, many [supplement] preparations on the market today have unknown origins and may contain un-identified amounts of monacolin … so only use these preparations under the guidance of a healthcare professional.” (Maas, p. 64-65).
I wonder if you’ve heard your midlife and older female clients talk about their rising cholesterol levels? Perhaps if you are in midlife, you’ve noticed this increase too? I know that I certainly did.
Why does cholesterol increase during and after menopause? And is there anything that we could be coaching our clients on to help them understand how to work with their Doctor to reduce the risk of higher cholesterol in post-menopause?
These were the questions that I’ve had to ask myself as well because numerous women in my programmes have noted that their Total and LDL-cholesterol has increased, and for many, despite going on Menopause-HRT.

Understanding Cholesterol:
The term ‘atherosclerosis’ is not a modern term. This word which describes the build-up of fatty-plaques in arteries, particularly the coronary arteries, was found in humans who lived thousands of years ago, before the spread of current risk factors. [Minelli et al, 2020]
For many decades, atherosclerosis was considered a degenerative disease, mainly determined by excess cholesterol and fat intake in the diet, however, these days, the theory of atherogenesis (the production of fatty-plaques), is based on dysfunction and inflammatory changes in the internal lining (the endothelium) of blood vessels.
Atherosclerosis is therefore, seen as a chronic inflammatory disease of large and medium-sized arteries, or endothelial dysfunction.
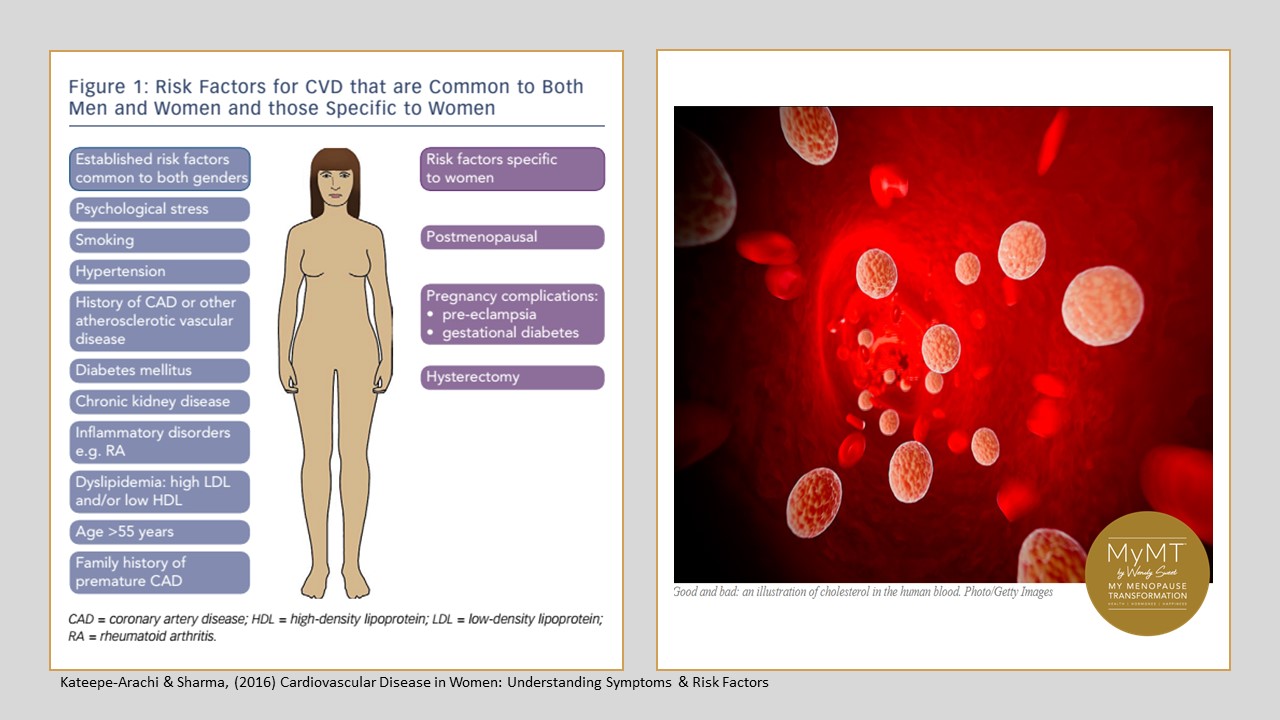
Numerous risk factors predispose your midlife and older clients to this endothelial inflammation, including 2familial history of cardiovascular disease, liver health (where cholesterol is made) diabetes mellitus, hypertension, cigarette-smoking, infections, older age (hence menopause is a risk), overweight and obesity status and any disorders of the blood clotting system.
Despite these underlying risk factors, the menopause transition is increasingly recognised as a time of life when cholesterol levels in the blood stream may increase. Explaining to your clients to get their blood pressure and cholesterol levels checked is therefore, sound advice!
Cholesterol is a molecule that combines with or dissolves in fats. The term for this is ‘lipophilic’.
We all need cholesterol and it is essential for human life because it has numerous roles that contribute to the function of cells. For example, cholesterol is an important component of the cell membrane, not only contributing to the structure of the cell membrane, but it also helps to regulate fluid shifts in and out of cells.
Cholesterol also functions in the synthesis or production of:
- Vitamin D,
- Steroid hormones (e.g., cortisol and aldosterone and adrenal androgens), and
- Sex hormones (e.g., testosterone, oestrogens and progesterone).
Cholesterol is also a constituent of bile salt used in digestion to facilitate absorption of the fat-soluble vitamins A, D, E, and K.
Many of you may have had your cholesterol levels checked over the years, and you will know that your blood work reports cholesterol markers as HDL, LDL, VLDL and Total Cholesterol.
High-density Lipoprotein (HDL), Low-density Lipoprotein (LDL), Very-Low Density Lipoprotein (VLDL) are all lipoprotein particles that transport cholesterol through the blood along with triglycerides (fatty acids combined with a glucose molecule).
These lipoproteins can be detected in the clinical setting to estimate the amount of cholesterol in the blood. Hence, why women should be getting tested.
You can see that Cholesterol is an important molecule, so why does it rise during and after menopause, which in some women, increases their risk for cardiovascular disease, including atherosclerotic changes in the arteries?
Well, if we want to answer this question, then we can’t go past the liver – afterall, this is the main site of cholesterol production in the human body.

The liver makes all the cholesterol your body needs, but during the menopause transition, the liver is ageing and changing in structure and function. (Brady, 2015).
Combined with the effects of declining oestrogen, which normally play an important role in the regulation of the total cholesterol level by reducing LDL (commonly called the ‘bad’ cholesterol) and increasing HDL (the ‘good’ cholesterol), cholesterol production can go a bit awry during menopause.
But there are other influences on cholesterol production during menopause too. While a woman’s diet, generally gives her liver all the cholesterol she needs for production, (100% of cholesterol comes from building blocks in the diet), other factors include:
- insomnia (therefore, the liver doesn’t get a chance to heal and detoxify overnight)
- stress (which uses up cholesterol to make more of the stress hormone cortisol)
- overweight and obesity status
- dietary influences, e.g. higher processed foods, high fat intake and high intake of animal proteins (which may be too high in cholesterol for an ageing liver)
- vegetarian or vegan status, whereby women may not be having enough cholesterol to help make hormones
- Fatty liver disease
- high alcohol intake (which affects the ageing liver enzymes)
In light of the changes to cholesterol production during and after menopause and a woman’s increased risk for inflammatory changes in her arteries, which in turn can contribute to atherosclerosis, my top-tips for you to help your clients with LDL and HDL cholesterol management during menopause are below.

- Get your clients to get their heart markers and cholesterol tested.
- Add celery and red yeast rice to their diet. Have some caution with red yeast rice supplements however, as they may have contaminants in them. (Maas, 2020) Food is best.
- Focus on liver detoxification pathways (how to do this is in the MyMT™ Health Practitioner Course – pre-register for January).
- Increase OATS in the diet. These contain beta-glucans which help to reduce LDL-Cholesterol>
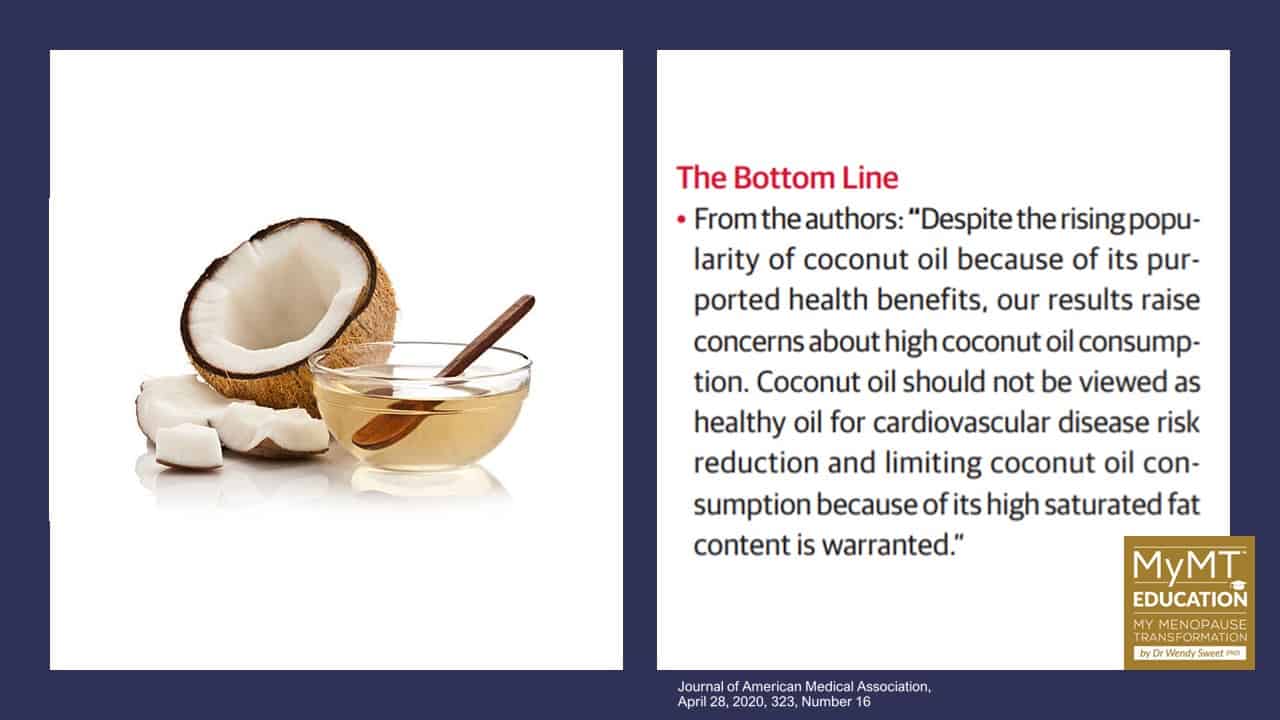
- Be careful of coconut oils. Refer statement below.
- Talk to your clients about their aerobic exercise (30 minutes minimum for at least 5 days a week). This is known to increase the ‘good’ HDL-cholesterol, which binds to harmful LDL-cholesterol and assists in the excretion pathways.
- Talk to your clients about alcohol consumption. Alcohol can contribute to raised triglycerides (blood fats) and cholesterol in the blood. If triglyceride levels become too high, these can build up in the liver, which is ageing, causing fatty liver disease. With these changes to liver function, the liver finds it harder to reduce or remove cholesterol from the blood.
- If clients are overweight, then help them to lose excess fat, especially visceral fat. How to achieve this is in the MyMT™ Menopause Weight Loss Coach Course.
References:
Brady CW. Liver disease in menopause. World J Gastroenterol. 2015 Jul 7;21(25):7613-20. doi: 10.3748/wjg.v21.i25.7613.
Currie, H., & Williams, C. Menopause, Cholesterol and Cardiovascular Disease, US Cardiology 2008;5(1):12–4. https://doi.org/10.15420/usc.2008.5.1.12
Huff T, Boyd B, Jialal I. Physiology, Cholesterol. [Updated 2023 Mar 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan
Khoudary, S., Aggarwai, B., Beckie, T., et al (2020). Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association. Circulation, 142: e506–e532
Kim IH, Kisseleva T, Brenner DA. Aging and liver disease. Curr Opin Gastroenterol. 2015 May;31(3):184-91.
Kooti W, Daraei N. A Review of the Antioxidant Activity of Celery ( Apium graveolens L). (2017). J Evid Based Complementary Altern Med. 22(4):1029-1034. doi: 10.1177/2156587217717415. Epub 2017 Jul 13.
Maas, A. (2019). A woman’s heart. why female heart health really matters. Great Britain: Aster Publ.
Minelli S, Minelli P, Montinari MR. Reflections on Atherosclerosis: Lesson from the Past and Future Research Directions. J Multidiscip Healthc. 2020;13:621-633
Nunes VS, da Silva Ferreira G, Quintão ECR. Cholesterol metabolism in aging simultaneously altered in liver and nervous system. Aging (Albany NY). 2022 Feb 7;14(3):1549-1561.
Tang, G. Y., Meng, X., Li, Y., Zhao, C. N., Liu, Q., & Li, H. B. (2017). Effects of Vegetables on Cardiovascular Diseases and Related Mechanisms. Nutrients, 9(8), 857. https://doi.org/10.3390/nu9080857


