The email arrived over the weekend. The lady works north of Perth in the mines. “I’m really concerned about my sleep” she mentioned. “I work shifts in the mines and shift work is wrecking havoc on my sleep patterns. My hot flushes seem worse, even though it’s winter, so I’m already dreading summer when it arrives.”
Hormones play a major role in regulating our behaviour and our physiology. As women move into their midlife menopause transition, many don’t think about the fact that the effectiveness of these hormones is dependent on time-based circadian patterns of production and secretion.
Nor do women who have physical jobs, think about the influence of not sleeping on their muscle health as they move through menopause. New research (Juliana et al, 2023), suggests that there is a skeletal muscle circadian clock and this plays a vital role in both lipid (fat) and glucose metabolism.
Therefore, when women aren’t sleeping in menopause, and they are watching the clock ticking away, this has a resultant effect on the musculo-skeletal system. It’s as I often say to women on my programmes who love their exercise, as I do too, “if you aren’t sleeping, then your muscles aren’t recovering from all of that exercise.”
It this is you or if you are a Health Practitioner or Personal Trainer and your clients are affected by aching muscles, sore joints and insomnia, then it’s time to think about the remarkable relationship between the circadian rhythm, menopause symptoms and muscles.
Many of us have also sought medical support for our symptoms in menopause, which is an appropriate action, but I wonder if the role of your circadian rhythm on your hormones and your muscles and bones even got a mention?
Judging by the thousands of women who have joined me over the years on the MyMT™ programmes, and my own experience, I assume not. That’s why, in this article, I wanted to draw your attention to the powerful relationship between the circadian rhythm and menopause symptoms.
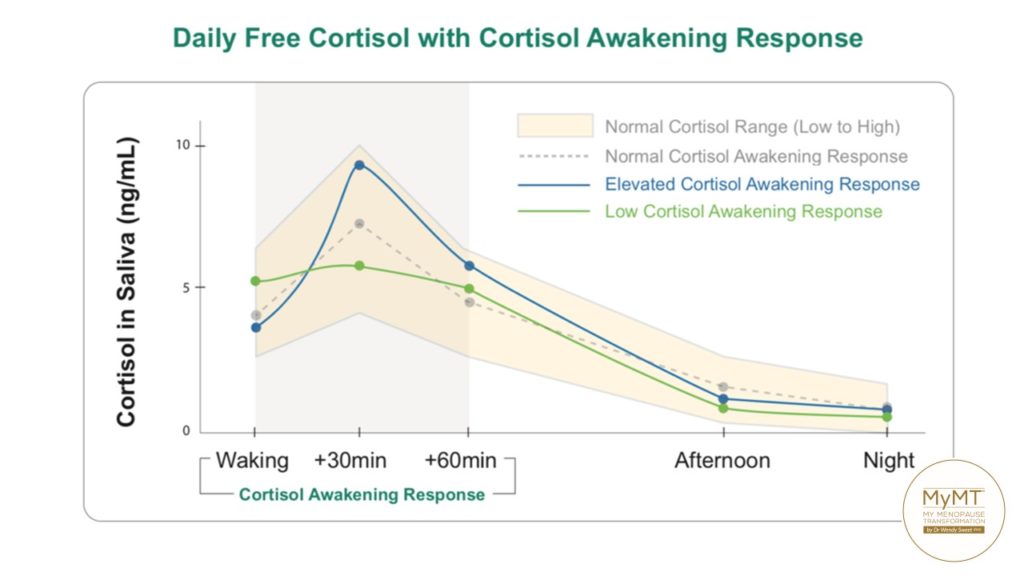
For women transitioning menopause who already suffer from insomnia, adjusting to the clock shifts with either shift work or daylight savings can be a tough gig. Simply because many women already have disrupted sleep patterns causing the chronic stress hormone, cortisol to be out of its normal daily pattern as well. This too impacts muscle health and recovery from exercise.
If your clients are experiencing hot flushes or waves of heat on awakening, which have got worse with shift work or changes to their exercise routines, then this may be due to elevated cortisol (a chronic stress hormone) levels throughout the night.
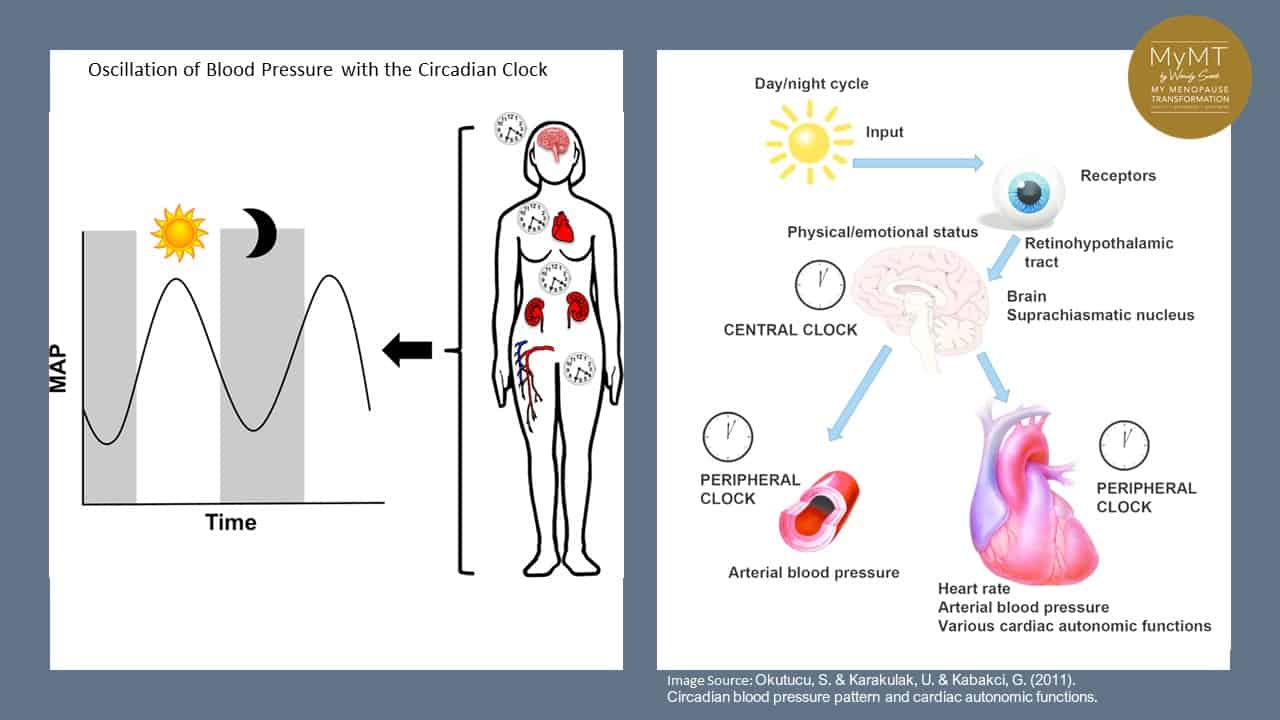
These elevated levels of cortisol and a disrupted circadian rhythm can contribute to higher blood pressure throughout the night (non-dipping) and first thing in the morning. This phenomenon is known as the Cortisol-Awakening Response. For those of you who have done my Practitioner 12 week course, I want to bring this back to your attention!
What is Overnight non-dipping Blood Pressure?
First described in 1988, the night time dip has become an accepted measure of cardiovascular risk. The ‘dip’ is defined as the difference between the mean systolic pressure in the day and mean systolic pressure during the night.
Over the years, research has shown that poor sleep quality, sleep curtailment, and sleep disorders (e.g., sleep apnea) are linked with BP ‘non-dipping’ overnight and a surge in blood pressure in the morning.
Hence, if your clients are experiencing extreme hot flushes in the morning on awakening, then you might want to talk to them about getting their blood pressure checked.
It’s also why I encourage women to consider their blood pressure management if they want to sleep all night. Even if women are on menopause HRT, this is an important consideration in their approach to lifestyle changes during and after menopause.
In humans, almost all behavioral and physiological functions occur on a rhythmic basis.
This is known as our circadian rhythm. Many of you who have been engaging with my other newsletters, will have heard me talk about this daily rhythm before. This daily circadian rhythm is driven by hormones. So, with reproductive hormones changing in peri-menopause and menopause, the circadian rhythm gets out of balance, thereby influencing menopause symptom chaos, including sore, aching muscles and joints.
The term ‘Circadian’ means “about a day” so circadian rhythms are daily fluctuations in human biology that can become messed up as women transition through menopause.
This internal clock, which gradually becomes established during the first months of life, controls the daily ups and downs of biological patterns, including body temperature, blood pressure, and the release of hormones that help our body to stay in balance.
Given that nearly all hormones (including reproductive hormones) play a key role in the cross-talk between different systems in the body, when the circadian rhythm gets out of balance (as in both menopause and daylight savings adjustments, or with shift work or staying up late, night after night) the rhythmic release of these hormones changes too.
Scientists now know that this altered pattern of hormonal release may contribute to the pathophysiology of a wide range of human disorders, especially during ageing. [Urbanski, 2011].
These disorders include high blood pressure and altered cardiovascular effects, altered immune function, altered behaviour associated with seasonal affective disorders such as eating disorders and mental health disorders.
For shift workers, such as the mine-worker in Australia who emailed me, not only are menopause hormonal changes challenging enough for sleep disruption, but so too is the added effect of shift work. The accumulation of both of these factors, has an impact on blood pressure and the function of numerous organs, including muscle and bone health.
Helping your clients towards deep, restorative sleep (between 2-4am), is important to reduce their heat fluctuations and night sweats too. When we sleep more deeply, blood flow is directed less toward the brain, which cools measurably. This is a good thing, because temperature regulation mechanisms are situated in the brain and for the brain to recover overnight, then the body needs to be cooler.
Deep sleep is an important factor in day-to-day recovery. Deep sleep patterns mean that the pituitary gland releases a pulse of growth hormone that stimulates tissue growth and muscle repair.
If women are lying awake night after night AND they are regular exercisers, this release of growth hormone does not reach the threshold it needs to for healing and repairing the body, including the healing of the gut, joints, bones and muscles.
This is also why I hear from so many women who are avid exercisers and they don’t understand that their sore muscles and joints are due to not just declining oestrogen, but also to not sleeping!
The image below is Sarah from Perth, who is now a MyMT Affiliate Practitioner. Helping her understand that her athletic performance with surf-lifesaving was dependent on sleep and not her training, meant that she took some time off from competing to get her sleep under control. I’m so pleased that she did, because what a comeback she made!

When reproductive hormones change during a woman’s menopause transition, this causes disruption to the normal circadian rhythms. Which is why, as women transition into or through menopause, it’s really important to restore this biological rhythm and make lifestyle adjustments to restore sleep!
Doing this helps to reduce overnight blood pressure as well as cortisol and insulin levels. As such, sleeping all night is the start to managing menopause symptoms.
If women don’t do this, then over time, their brain and organs get out of balance. Then the 2-3am ‘awake’ period becomes ‘normalised’. When women restore their sleep, they restore their energy levels, their joints heal and their hot flushes and night sweats reduce too.
Furthermore, if women are overweight, they too must focus on their sleep routines. This is because fat cells and the role of lipase, an enzyme which breaks down fat and releases it from fat cells, functions on a 24 hr circadian cycle.
Scientists who research lipid (fat) disorders, know that circadian clock disruption, causes disruption of the metabolism and transport of fats and proteins, and this disruption may be responsible for the development of a large spectrum of health problems, ranging from cardiovascular diseases, to metabolic syndrome, even to cancer development. [Gnocchi, Pedrelli et al., 2015]
As I often mention in my workshops and online courses, when we’ve been waking up night after night, then our brain and body reads this as our ‘new normal’. But this is what leads us down the path towards the build-up of inflammation in our cells and tissues.
Not sleeping is now recognised as one of the main contributing factors to changing health as women move into their post-menopause years. This is concerning, especially in light of the high rates of heart disease in post-menopause women.
The United Kingdom, Australia and New Zealand have some of the highest incidence of post-menopause heart disease globally. America is up there too.
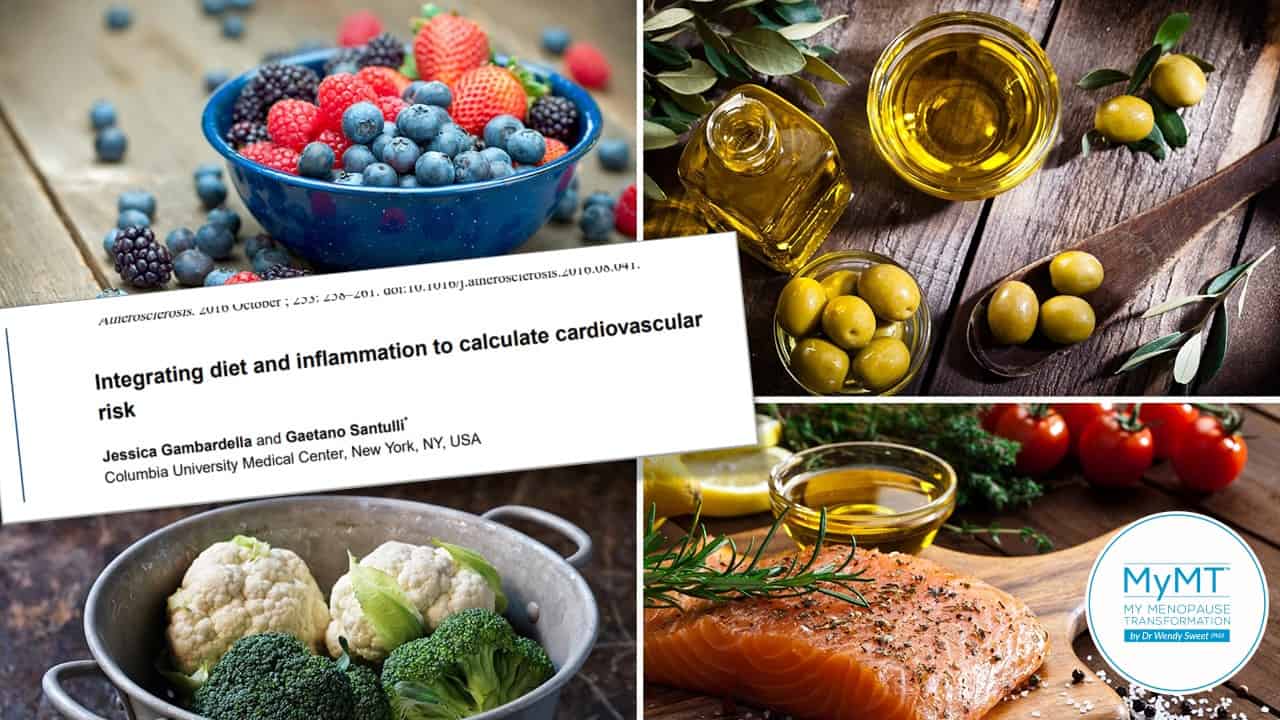
But here’s the thing – if women aren’t sleeping, the heart and immune system stay under stress all day long, particularly, when if women are regular exercisers or they have busy, stressful jobs or home environments. This causes more inflammation in cells and tissues and in ageing research, is known as oxidative stress or ‘inflammaging‘.
It’s why one of the main dietary changes that we can make, no matter where we live in the world, is to move towards a more Mediterranean Style dietary approach.
Ageing is typically associated with impairments of the circadian rhythm and a natural decrease in melatonin (sleep hormone) secretion. Menopause is the natural transition into our ageing, and whilst many of us still feel young as we enter this phase of our life, inside our body there are powerful inflammatory changes occurring, especially if women aren’t sleeping well.
Understanding how to slow these changes down using evidenced lifestyle strategies is important. When we do, we can help clients to resolve their symptoms, lose weight, improve mood and feel fabulous in their fifties.
Many women go on menopause HRT and/or anti-depressants, which helps them enormously (and I don’t interfere in any medications women are on, because this is between you and your Doctor), but I am passionate about women also understanding the lifestyle-science solutions that can be easily put into place too.
This is what my 12 week Practitioner programme teaches you to focus on. My next course starts this week and I’m excited to meet new Practitioners to help them understand the lifestyle science behind managing menopause symptoms.
I hope you can join me one day too. And don’t forget the 6 week MyMT™ Weight Loss Coach Course and a brand new 3 week Introduction to the Science of Menopause Course for Health Coaches.
Dr Wendy Sweet (PhD)/ Founder: MyMT™/ Member: Australasian Society of Lifestyle Medicine.

References:
Davis, S., Castelo-Branco, C. et.al. (2012). Understanding weight gain at menopause. Climacteric, 15: 419–429.
Geddes, L. (2019). Chasing the Sun: The new science of sunlight and how it shapes our bodies and minds. London: Profile Books.
Gnocchi D, Pedrelli M, Hurt-Camejo E, Parini P. Lipids around the Clock: Focus on Circadian Rhythms and Lipid Metabolism. Biology (Basel). 2015 Feb 5;4(1):104-32.
Harvard Health Report (2017). Improving Sleep. Harvard Health Publication
Jehan, S., Giardin, J-L, Auguste, E., et al (2017). Sleep, Melatonin and the Menopausal Transition: What are the links? Sleep Science, 10(1): 11-18.
Juliana N, Azmi L, Effendy NM, Mohd Fahmi Teng NI, Abu IF, Abu Bakar NN, Azmani S, Yazit NAA, Kadiman S, Das S. Effect of Circadian Rhythm Disturbance on the Human Musculoskeletal System and the Importance of Nutritional Strategies. Nutrients. 2023 Feb 1;15(3):734. doi: 10.3390/nu15030734.
Reinke H. & Asher G. (2017). Circadian clock control of liver metabolic functions. Gastroenterology, 150: 574–580.
Rizzi, M. et al. (2016). Sleep Disorders in Fibromyalgia Syndrome. Journal of Pain Relief, 5:2, 1-5
Sharma, S. & Kavuru, M. (2010). Sleep and Metabolism: An Overview. Int. Journal of Endocrinology, Article ID 270832, 1-12.
Urbanski HF. Role of circadian neuroendocrine rhythms in the control of behavior and physiology. Neuroendocrinology. 2011;93(4):211-22. doi: 10.1159/000327399.
Woods, N. et al. (2009). Cortisol Levels during the Menopausal Transition and Early Postmenopause: Observations from the Seattle Midlife Women’s Health Study. Menopause, 16(4): 708–718.



