The evenings are rather long in Scotland at the moment. I know this because I’ve been emailing Monique who lives in a castle right at the tip of Scotland. It is light until at least 10pm and for women in menopause who aren’t sleeping that’s not a good thing at all. This time last year, I was in Scotland – oh my, how much has changed in the world since then! When I asked who wasn’t sleeping all night, over 150 women put up their hands … and yes, it’s a similar story no matter where I’ve presented my seminars – menopausal women united in mid-life insomnia! I get quite concerned about this, because menopause-related insomnia is not only exhausting us but for many women it’s sending them into a downward spiral into health choas with auto-immune changes (fibro-myalgia), belly-fat weight gain (central adiposity), heart palpitations and for many women, night sweats and hot flushes too.

That’s why if we are going to feel healthy as we move through mid-life, we need our sleep.
When I visited Edinburgh last year, I told the women their geographical location living in the far north of the UK, needs to be managed. Especially now, during summer. Long summer evenings don’t bode well for getting off to sleep. Longer hours of daylight mess up our natural circadian rhythm and when this happens, then our menopause symptoms and health become worse. Hence, drawing the curtains earlier and ensuring that bedrooms are as dark as possible, matters. So, too does keeping the bedroom cooler than normal.
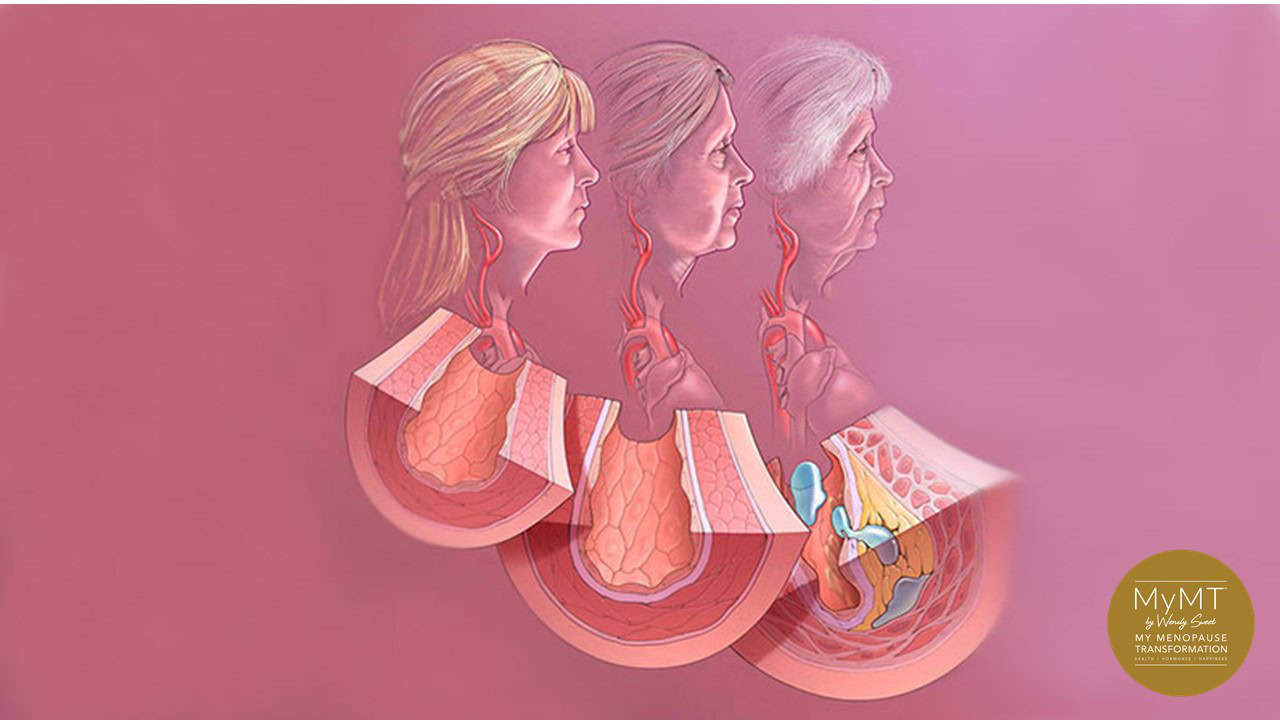
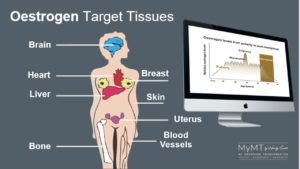
When we don’t sleep, we experience changes in our overall health and wellbeing. I think we all already know this. But did you know that just going into and through menopause, means that our changing oestrogen levels interfere with our sleep quality and quantity as well. If we aren’t sleeping between the hours of 2-5am, then we aren’t getting our precious deep, recovery sleep. The body needs sleep as much as it needs awake time and the reason for this, is that when we sleep we heal our immune system as well as our heart.
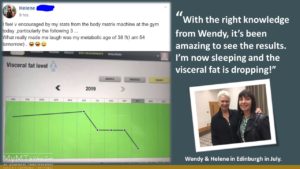
When women come onto the MyMT™ programmes, the very first module they listen to is how to sleep all night. It’s the foundation of turning around our symptoms in menopause. Sharing knowledge about our menopause transition is what I’m so passionate about and having a room-full of mid-life women to talk to fills me with gratitude. And how cool was it that Isobel and Helene were there with me too? Both have been on the MyMT™ programmes and it was such a privilege to have them come along and for me to meet them in person. When Isobel said she was still struggling a bit with her sleep, I knew she was listening when I spoke about how our geographical location is often against us when we go into menopause. It’s the same for women living in the deep-south of New Zealand – they have longer evenings in summer too.
That’s why I was so delighted to get this message from Isobel this morning.
“Everything you have put together in this programme is perfect for me. I went home from your talk, drew the curtains and resolved to sleep through the night with your suggestions. I used to wake up and have a cup of tea and read at 3am as well as get up to use the bathroom. But I now understand that this isn’t helping my health. I also play a lot of tennis, so my muscles aren’t recovering. Well, I’m happy to report that I have slept right through for 2 nights!”
When we all lead such busy lives, it’s so important to get our sleep sorted as we move into menopause. I can’t reiterate this enough. As I often mention to women, when we have been waking up night after night, then our brain and body reads this as our ‘new normal’. But this is what leads us down the path towards worsening inflammation in our cells and tissues as we age.
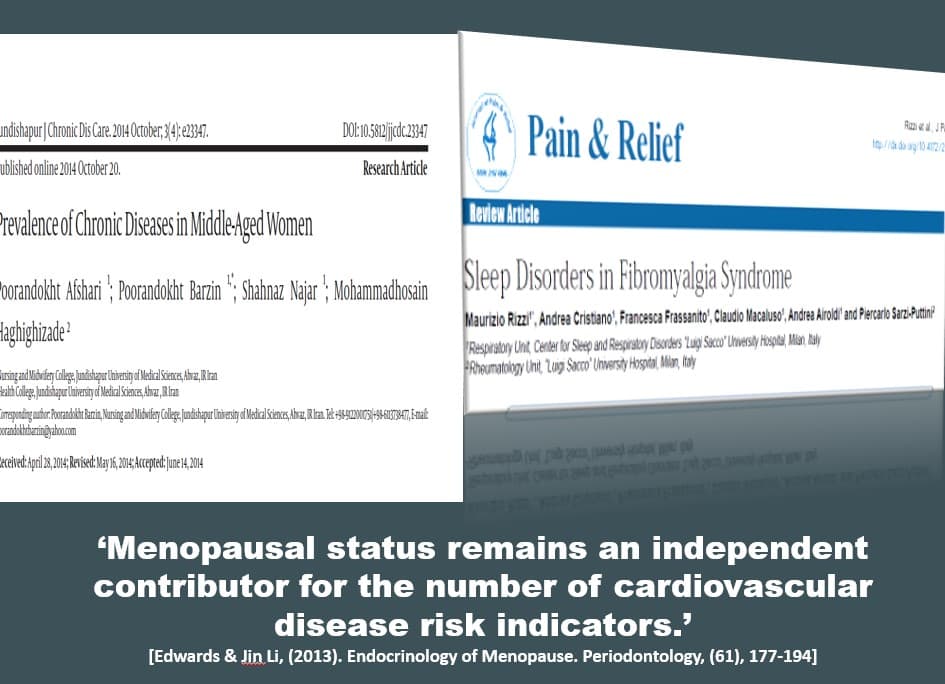
Not sleeping is now recognised as one of the main contributing factors to changing health as we move into our post-menopause years, contributing to heart disease as well. The United Kingdom, Australia and New Zealand have some of the highest incidence of post-menopause heart disease.
If we aren’t sleeping, our heart and immune system stay under stress all day long, particularly, when we are regular exercisers or we have busy, stressful jobs or home environments. That’s why I love getting women sleeping all night. It helps to reduce their worsening symptoms in menopause. And yes, your diet is important in this too. Over the past week in my private coaching groups, I’ve been having a focus on the scientific evidence between sleep quality and dietary nutrients.

How does our body heal overnight?
The human immune system and sleep are both associated and influenced by each other. That’s why sleep deprivation makes our body susceptible to many infections. But for women in menopause, there is another added factor. As I mention in my seminars (now available online for you), menopause is the biological gateway to our ageing years, and as such, we have changes related to ageing going on all around our body.
This includes our immune system which is under programmed senescence. This is the term which describes programmed biological ageing. Think of autumn leaves discolouring and falling from a tree. This is an example of programmed senescence in plants. Because we are ageing, our immune system is too and as such, it doesn’t produce as many immune-fighting lymphocyte cells in our bone marrow. When we don’t sleep, we are behind the eight-ball with our immune health even more.
Sleep deprivation makes a living body susceptible to many infectious agents too – a concern for all of us within the context of this pandemic.
Have you ever wondered why we are programmed to sleep? I become curious about this when I wasn’t sleeping during menopause either. Sleep deprivation was so furstrating. I knew that my body wasn’t healing and recovering overnight and not sleeping was leaving me too exhausted to recover from the exercise I love to do. At the time, I also didn’t understand that not sleeping was blocking fat-loss mechanisms overnight and causing increased hot flushes too because blood pressure and cortisol remain higher during the day when we don’t sleep. Cortisol that does not follow the normal pattern can trigger blood sugar imbalances, food cravings and fat storage, especially around the middle.
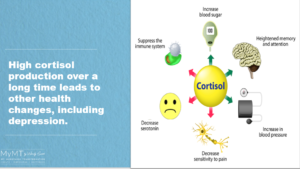
I talk a lot about cortisol during my seminars. As we move into menopause, it’s this hormone which needs to be settled down.
Cortisol is one of our chronic stress hormones and it’s important to women in menopause who aren’t sleeping, because it works in synergy or partnership with our sleep hormone melatonin. If cortisol levels are too high when we go to bed, then we don’t produce enough melatonin to keep us asleep for the healing hours between 2-4am.
Then if melatonin levels are lower than normal, we either can’t get off to sleep or we wake up in the night or we don’t sleep deeply enough to have the restorative sleep that we so need to keep our energy levels up for all that we do in our day.
“Our capacity to remain healthy is badly affected by loss of sleep and sense of comfort” reports researchers who have looked at the role of sleep on the immune system. They go on to state that our white blood cells, called leukocytes, don’t reach the levels that they should due to lack of sleep and this makes us vulnerable to sickness, flu and immune system health changes. For women in menopause, this may also lead to the autoimmune problem of fibromyalgia.
When we don’t sleep and our sleep-wake cycle is affected, then our nervous system is also affected leaving us feeling more anxious and ‘wired’. Overnight our nervous system and immune system work together – this is why when women are going through menopause and are waking up night after night, they feel wired, they feel hotter than normal and their muscles and joints remain sore or they put on weight. In other words they remain ‘inflamed’ but many, like Lucinda, then become frustrated when exercise doesn’t help them to lose weight but leaves them injured instead. Read her story HERE.

The build-up of inflammation in the body not only makes our symptoms worse, but the increased cortisol that arrives from the body trying to reduce inflammation, can leave us lower in progesterone as well. Then of course, there is the additional inflammation from our biological ageing. That’s why I talk about a relatively new term in ageing science, called ‘inflammaging’.
I first heard this term at ageing conferences I was attending as part of my doctoral studies. ‘Inflammaging’ refers to chronic, low-grade inflammation that characterises ageing. And as I keep reminding women, even though we feel young, inside our body our cells are ageing. The more rapidly they age and acquire inflammatory changes, depends on the lifestyle we’ve lead for years, the amount of exercise we do (too much or too little), our diet and of course, whether or not we are sleeping. When inflammation builds up several tissues and organs acquire chronic inflammation, including the gut microbiota.
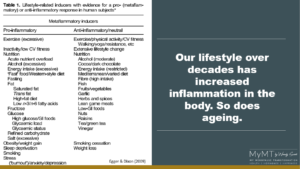
Professors Garry Egger and John Dixon show the characteristics of both pro and anti-inflammatory influences and I show this slide in my online Masterclass on Menopause too. From an evolutionary perspective, a variety of stimuli keep us in the ‘inflammaging’ cycle and I include menopause-related hormone changes in this too. As Professor Egger states, “We have been operating in silo’s. We haven’t been taking into account all the other effects on inflammation, including ageing.”
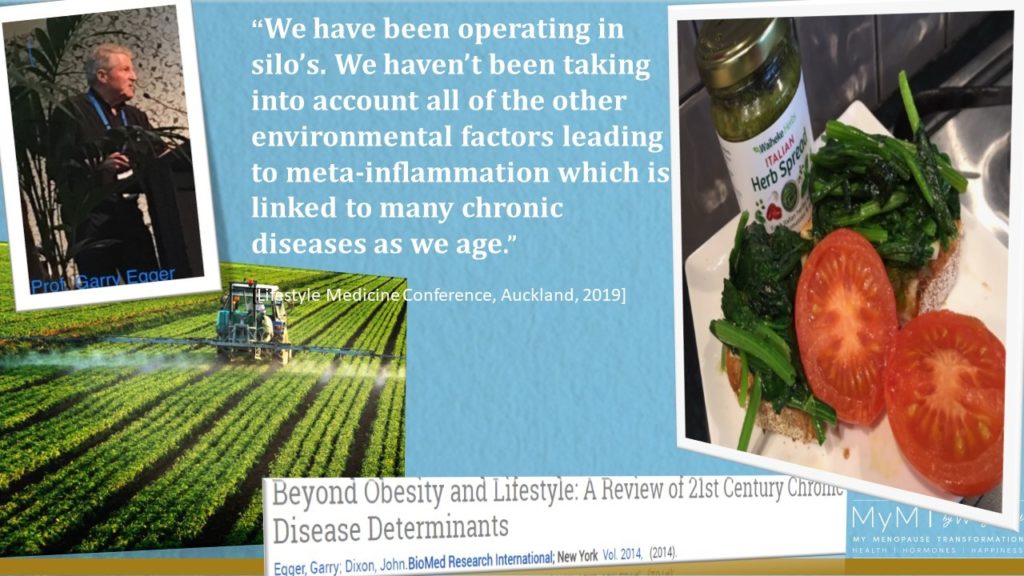
For women coming to join me on the online MyMT™ programmes, I coach them how to manage their inflammaging. The strategies to sleep all night are fundamental to this as is improving liver, gut and joint health. As well, the dietary approach I use focuses on specific nutrients that help to reduce inflammation in our body as we age. This includes foods such as beets and celery, which help to improve blood pressure and blood vessel dilation.

I can’t wait for you to join me too. With over 2000 women now having gone through this fabulous online lifestyle-change programme in over 25 countries, it would be my privilege to support and guide you. If you are thinner or leaner, then the Circuit Breaker programme is for you, otherwise the weight loss Transform Me programme is the one to choose. Both programmes are on savings of NZ$50 at the moment, making these online 12 week courses, NZ$349 [approx. AUS$317/ UK£165/ US$206.] All programmes have a monthly payment option. Use the promo code JOIN MYMT to access your savings.
When my own symptoms overwhelmed me, I knew that women in menopause were forgotten when it comes to how to turn around symptoms and improve our health as we age. That’s why I designed MyMT™ – it’s the only programme that focuses on the integration of ALL of the solutions that we need to put into place to prevent changing health from menopause-related changes as we age. I hope you can visit the website when you have time.

Dr Wendy Sweet, PhD/ Women’s Healthy Ageing Researcher & MyMT™ Lifestyle Coach. Member: Australasian Society of Lifestyle Medicine
References:
Asif N., Iqbal R., et. Al. (2017). Human immune system during sleep. American J. Clin Exp Immunol.,6 (6):92-96
Egger, G. & Dixon, J. (2009). Obesity and chronic disease: always offender or often just accomplice. British Journal of Nutrition, 102, 1238-1242.
Franceschi, C. et al. (2018) Inflammaging: a new immune-metabolic viewpoint for age-related diseases. Nat. Rev Endocrinology, 14(10):576-590.
Theurey, P. & Pizzo, P. (2018). The Aging Mitochondria. Genes, 9(22), 1-13. doi:10.3390/genes9010022