What nutrients increase bone density?
It’s a question I asked myself over a year ago when my bone density scan showed early osteoporotic changes. Over 30 years of high levels of activity as well as not understanding how to change my lifestyle to match my menopause transition had caught up with my bone health.
With osteoporosis affecting one out of three post-menopausal women, their remaining lifetime risk of fragility fractures exceeds that of breast cancer, mentioned a 2014 review of nutrition and bone health in women after menopause (Rizzoli et al, 2014).
Menopause is the biological gateway for these changes to occur, hence I think that this is a wake-up call for all of us, don’t you? It certainly was over a year ago for me and I’m pleased to say that my latest bone density scan this week saw a ‘statistically significant’ improvement in my bone density … without medications. If you look at the graph on the banner above, that’s me. Moving upwards, not down.
Over the past month I’ve been focusing on nutrients that we need during menopause, and with bone density on my mind, I wanted to help you to focus on this too.
Approximately 60-80% peak bone mass is determined by genetics. And with bone health data out of America indicating that around 10 million Americans over the age of 50 have osteoporosis and another 34 million have low bone mass, thinking about our bone health matters during our menopause transition.
I think that we all know that healthy nutritional habits combined with exercise should be encouraged in order to maintain bone health, but what exactly does that mean? What type of food should we eat? What specific exercise should we do? (this is covered in my article on exercise) and of course, can we actually turn around our bone health as we age?
These are the questions that I was most interested in myself, so if you want to know about the essential nutrients for your bone health, then please have a read when you get time.
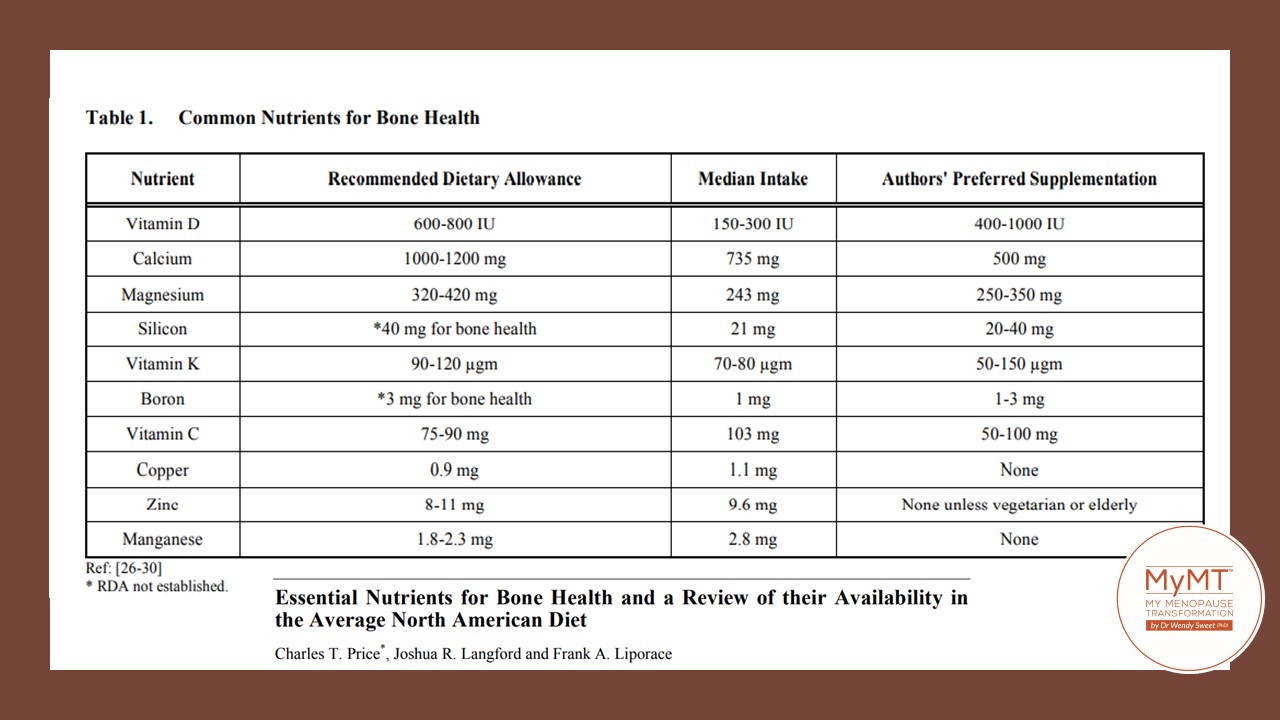
Numerous nutrients are needed for bone health, not ‘just’ calcium or Vitamin D. And yes, real food is better in terms of your absorption of these nutrients, rather than just supplements. So, let’s explore what nutrients and foods your beautiful, ageing bones need.
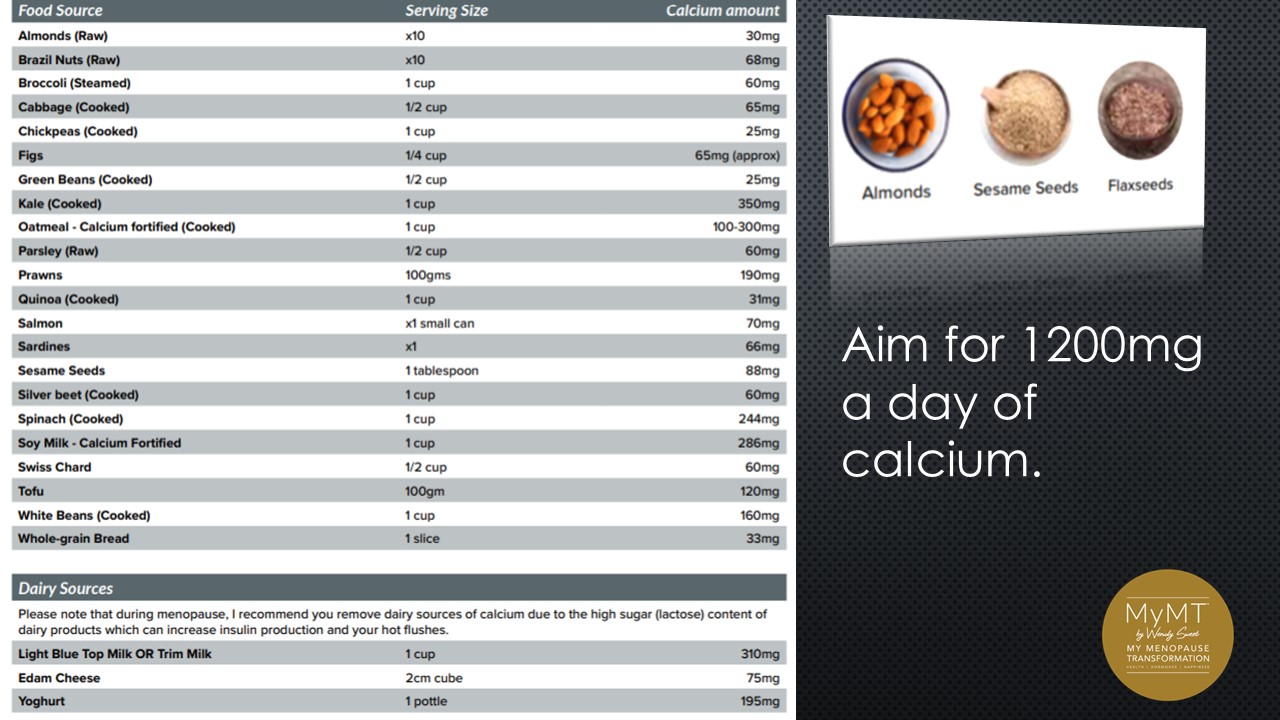
CALCIUM
800mg up to 1200mg a day, every day. If you are an exerciser and doing weights, then take the higher-amount approach. Calcium is a major component of muscle contraction and if you have restless legs, muscle cramps or muscle aches and pains, then explore your calcium intake.
Also be aware that emerging heart health research also suggests that food is better than supplements. (Rizzoli et al, 2014). And don’t forget that if you have GUT HEALTH concerns, then join me on the MyMT™ programmes as I have a module called ‘Restore your Grateful Gut’. If you already have IBS or other gut health concerns, then you may not be absorbing the Vitamin D you need in order for calcium to do its job.
Vitamin D is not just the sunshine vitamin – it is needed to help your gut absorb calcium. A deficiency decreases the amount of calcium absorbed from the intestine and this then increases the activity of the parathyroid hormone (PTH).
This hormone is activated to try and rebalance the decrease in serum (blood levels) of calcium by increasing calcium resorption from the bone. Vitamin D and Calcium work together to maintain strong bones.
EXTRA VIRGIN OLIVE OIL [EVOO]
On completing my bone density scan, the surprised Technician enquired as to how I had managed to improve my bone density status, “Extra Virgin Olive Oil” was my response. Looking surprised, she said she had no idea! But when women come onto the MyMT™ programmes, I introduce them to the Mediterranean Diet, which I’ve modified for women in menopause and post-menopause. There’s a reason for this.
The overall quality of the Mediterranean Diet is related to improved quality of life in women as they age and the intake of EVOO in numerous scientific trials, is that it generates health benefits, such as the prevention of cardiovascular diseases, the improvement of inflammatory markers in bone and improvements in the composition of the gut microbiota.
These benefits are attributed to the excellent nutritional composition of EVOO, which has a higher content, of mono-unsaturated fatty acids and minor compounds such as oleuropein and hydroxytyrosol. It is these dietary components that confer protection to our skeletal system against osteoporosis and the consumption of olives, olive oil and olive polyphenols has been shown to improve bone health (Kok-Yong Chin et al, 2016].

PROTEIN
Protein accounts for approximately 50% of bone volume and about 1/3 of its mass. Collagen helps in the process of building new bone cells and re-modelling bones through the modification of amino acids, which are the building blocks of protein and Vitamin C enhances the production of collagen as we age.
As I mention in my 12 week coaching programmes, we don’t need a lot of protein, but we do need a minimum of 0.8 – 1.0gm/kg/day and up to 1.2 to 1.4gm/kg/day for those who are weight training.
One of the main concerns that women have as they age, is whether to have meat sources of protein or plant proteins, but relatively new research suggests that a mix of dietary proteins is beneficial however, my caution to you is to watch the acid-load of the diet.
A high acid-load, places strain on your kidneys. For the body to be able to reduce the acidity, your bones and teeth leach calcium and phosphorus to re-stabilise the internal environment. In the Western world, the main contributors to the acid load from the diet are meat, fish, milk and dairy products, and eggs, followed by cereal grains.
Conversely, base-producing diets (alkaline diets), characterized by relatively higher intake of fruits and vegetables, are rich in organic anion salts that are metabolized to alkaline salts such as bicarbonate, which also helps your bones.
OTHER LESSER KNOWN NUTRIENTS FOR BONE HEALTH
Numerous vitamins and minerals are associated with our bone health independent of Vitamin D and calcium. These nutrients include Magnesium, Vitamin K, Silicon and Boron (Price et al, 2012).
Magnesium is often regarded as a nutrient which is helpful for managing hot flushes, (yes it is), but it is also necessary for helping with our ageing muscles, blood vessels and bones. In fact, I believe it is just as important as calcium for all of us.
A study of women with osteoporosis in Israel, reported significantly increased bone mineral density with 250mg of magnesium supplementation compared with a control group who did not take magnesium supplements. Dietary sources of magnesium include almonds, cashews, brown rice, peanuts, kidney beans, black-eyed beans and lentils.
Silicon is another important contributor to our bone health. Silicon deficiency is associated with poor skeletal development as it plays a role in the initiation of the mineralisation process. Dietary sources of silicon include whole grains, carrots and green beans.
Vitamin K has several different forms, but Vitamin K1 and K2 are the naturally occurring forms which we need because low Vitamin K impacts bone turnover and bone strength.
Whilst Vitamin K intake needs to be managed if women are on blood thinners, if you aren’t, then look at your sources of Vitamin K from kale, collard greens, fresh spinach, brussel sprouts, iceberg lettuce and prunes. You need a minimum of 90 micrograms daily.
As we age, it makes sense that we have a renewed focus on bone health. Nutritional needs for bone health can be met with proper food choices.
Women who are vegetarian or vegan as well as thinner and leaner must also be careful to monitor their nutrients as well as protein intake, especially if they are doing a lot of heavy lifting-type exercise.
The risk of osteoporosis and/or fragility fractures can be reduced through healthy lifestyle changes mentions a review of nutrition and bone health in women after menopause.
These changes include adequate dietary intakes of calcium, vitamin D, magnesium and protein, regular weight-bearing exercise (but not too much heavy exercise if you aren’t sleeping), reduction in alcohol intake and smoking cessation and of course, sleeping all night and turning around our gut health.
Furthermore, the European guidance for the diagnosis and management of osteoporosis in postmenopausal women recommends a daily intake of at least 1000 mg/day for calcium, 800 IU/day for vitamin D and 1 g/kg body weight of protein for all women aged over 50 years.
Hence, the review concluded that the development of programmes that encourage lifestyle changes (in particular balanced nutrient intakes) are therefore essential for the reduction of osteoporosis risk. (Rizzoli et al, 2014). I couldn’t agree more.
If you are ready to make that change, then have a listen to my video below, which explains my programmes. I hope you can join me sometime if you want to turn around your symptoms and/ or lose weight using the science of lifestyle medicine. If you are already on medications for menopause, then I don’t interfere with these as this is between you and your Doctor.
Dr Wendy Sweet (PhD) MyMT™ Founder & Member: Australasian Society of Lifestyle Medicine.
References:
Chin KY, Ima-Nirwana S. Olives and Bone: A Green Osteoporosis Prevention Option. Int J Environ Res Public Health. 2016 Jul 26;13(8):755.
Lohana, C. & Samir, N. (2016). Risk Management of Osteoporosis in Postmenopausal Women. Global Journal of Health Science, Vol. 8, No. 11; 36-44
de Villiersa, T. & Goldstein, S. (2021). Update on bone health: the International Menopause Society White Paper 2021. Downloaded from: https://www.imsociety.org/education/world-menopause-day/#whitepaper
Rizzoli R., Bischoff-Ferrari H., Dawson-Hughes B., Weaver C. (2014). Nutrition and bone health in women after the menopause. Womens Health (Lond). 10(6):599-608. doi: 10.2217/whe.14.40. PMID: 25482487.
Rondanelli M, Faliva MA, Tartara A, Gasparri C, Perna S, Infantino V, Riva A, Petrangolini G, Peroni G. An update on magnesium and bone health. Biometals. 2021 Aug;34(4):715-736.
Shams-White M., Chung M., Fu Z., Insogna K., Karlsen M., et al. (2018). Animal versus plant protein and adult bone health: A systematic review and meta-analysis from the National Osteoporosis Foundation. PLOS ONE 13(2): e0192459. https://doi.org/10.1371/journal.pone.0192459
Sözen, T., Özışık, L., & Başaran, N. Ç. (2017). An overview and management of osteoporosis. European journal of rheumatology, 4(1), 46–56. https://doi.org/10.5152/eurjrheum.2016.048