Your Mitochondria Matter in Menopause!
Do you ever watch those programmes on TV that trace a person’s ancestry? Or perhaps you’ve had your own ancestry traced.
If so, then the ability to do this is thanks to your mother, grandmother, great-grandmother and so on and the number and size of tiny organelles called mitochondria.
A mitochondrial DNA test (mtDNA test) traces a person’s matrilineal or mother-line ancestry using the DNA in his or her mitochondria. mtDNA is passed down by the mother unchanged, to all her children, both male and female.
You may have heard about your mitochondria.
Especially if you’ve been following my posts for a while. After a number of conversations with women about their menopause brain fog this week, I was thinking about these mighty organelles and the link to brain health as you move into peri-menopause and through menopause.
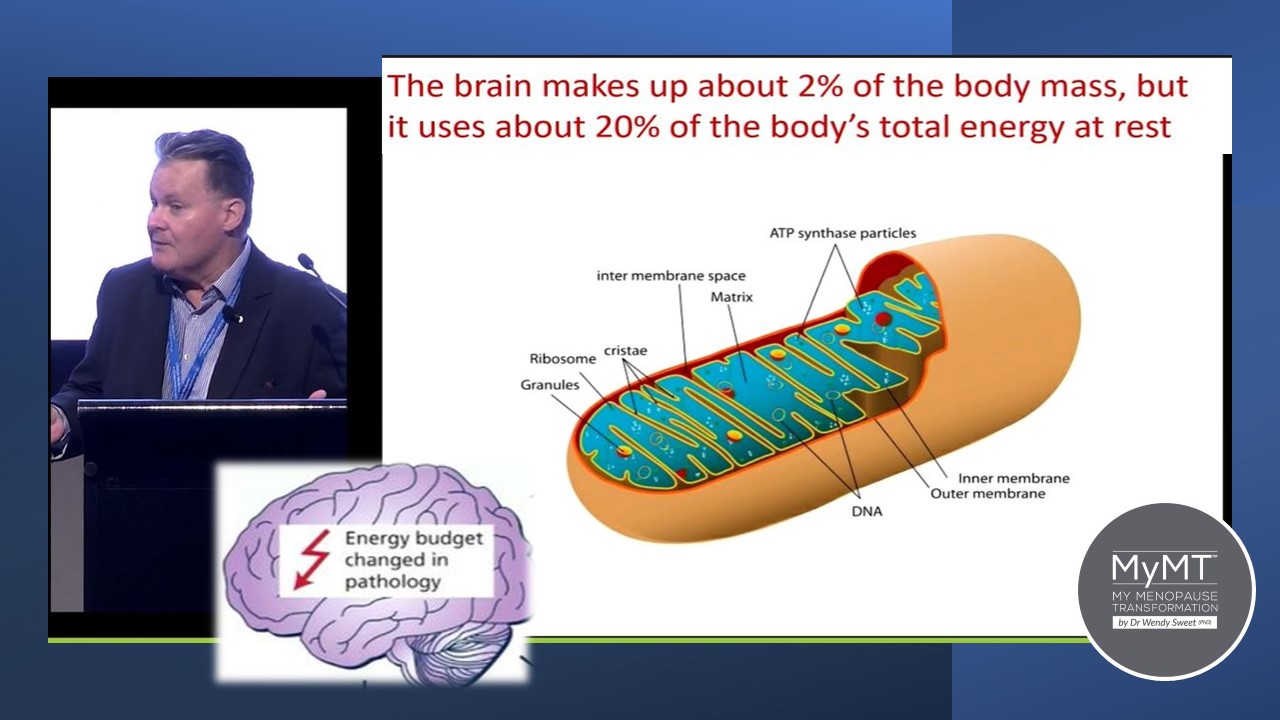
The major role of mitochondria is to convert dietary fuel into ATP – your energy molecule. Hence, mitochondria are found throughout your body, including in your brain tissue and nervous system pathways.
Our mitochondria are inherited from our mothers via the egg and genetic tracing can be used to trace ancestry from the maternal branches of families. When it comes to our health during menopause, we never think about the health of our mother when we were born do we?
But maternal health and their exposure to toxins over their lifetime influences your health as you move through your life too.
This is because the health and fitness of your mother when you were born, determines the baseline number and size of your mitochondrial cells throughout your body and brain.
Many women complain of forgetfulness around the time of the menopausal transition and because of the association between episodic memory loss and Alzheimer’s disease, this ‘forgetfulness’ symptom (aka brain fog) is of course worrisome.
However, forgetfulness is a common symptom at other important stages of a female’s life, including during puberty and pregnancy, when hormonal changes are occurring.
There’s a reason I’m talking to you about forgetfulness and your brain’s mitochondria.
Professor Zoltan Sarnyai (that’s him in the image below) is a neuroscientist researching mental illness at the Laboratory of Psychiatric Neuroscience at James Cook University in Australia. He’s a very clever guy.
It was his presentation at a Lifestyle Medicine conference that bought my attention to the link between our menopause hormonal changes, our brain-fog, our stress and our mighty mitochondria. Most importantly, he too, recognises that there are specific lifestyle solutions to help preserve the brains’ mitochondrial health with age, and to reduce brain fog during menopause.
Hormones and Mitochondria: The Science Behind Peri Menopause Brain Fog
There are millions of mitochondrial cells around the body and they have multiple and crucial roles in cell maintenance, survival and wellbeing. Most importantly, mitochondrial cells are where your energy is made.
Mitochondria also play an essential role in the generation of steroid hormones including the female sex hormones. As such, female sex hormones are, in turn, able to modulate mitochondrial activities. (Lejri et al. 2018).
We already know that a large amount of oestrogen in the female body is released from the ovaries. But as it’s released it circulates throughout the body, and crosses the blood-brain barrier to act upon the cells within the brain.
In the brain, oestrogen has a number of roles:
- it helps with cerebral blood flow
- it preserves and maintains nerve transmission.
- it acts as an anti-inflammatory agent.
This is why our menopause transition becomes a perfect storm for disruptions to our brain function and cognition. Oestrogen acts directly upon mitochondria in the brain. (Del Río et al., 2018).
It makes sense then, that as women move through menopause, our brain mitochondria are affected in ways that promote inflammatory changes and nerve transmission may therefore, be disrupted.
Which is why, it’s no surprise that our entry into peri menopause, the stage before our periods end, increases the incidence of forgetfulness and brain-fog.
And as Professor Sarnyai reminds us, stress (both current and past), has a long-lasting and negative impact on brain mitochondria.
Lifestyle Solutions for Managing Menopause Brain Fog
High levels of daily stress, including not sleeping, creates higher levels of inflammation in the brain’s mitochondrial cells. These inflammatory changes may lead to a number of symptoms, including:
- fatigue
- brain fog and depression
- memory loss, lack of motivation and feelings of over-whelm
- pain and soreness in muscles
- headaches and migraines
- poor sleep
Do any of these symptoms sound familiar to you now that you are in or past your menopause transition?
This is what Professor Sarnyai reminded me about – the link between our ageing mitochondria and inflammatory changes and why we have to look after our brain, not only throughout our life, but also, during and after menopause.
Whether you have chosen to go on menopause HRT or not, there are specific lifestyle solutions you can implement too. I will tell you about these below, so please keep reading!
What can I do to reduce my menopause brain fog with lifestyle solutions?
- Manage your stress – “whatever happens with stress in the brain, happens to the body” mentioned Professor Sarnyai. It’s a reminder that focusing on strategies to manage stress is important, including physical stress from over-exercising. If you are doing too much high intensity exercise day after day, then this can cause over-loading on your nervous system too.
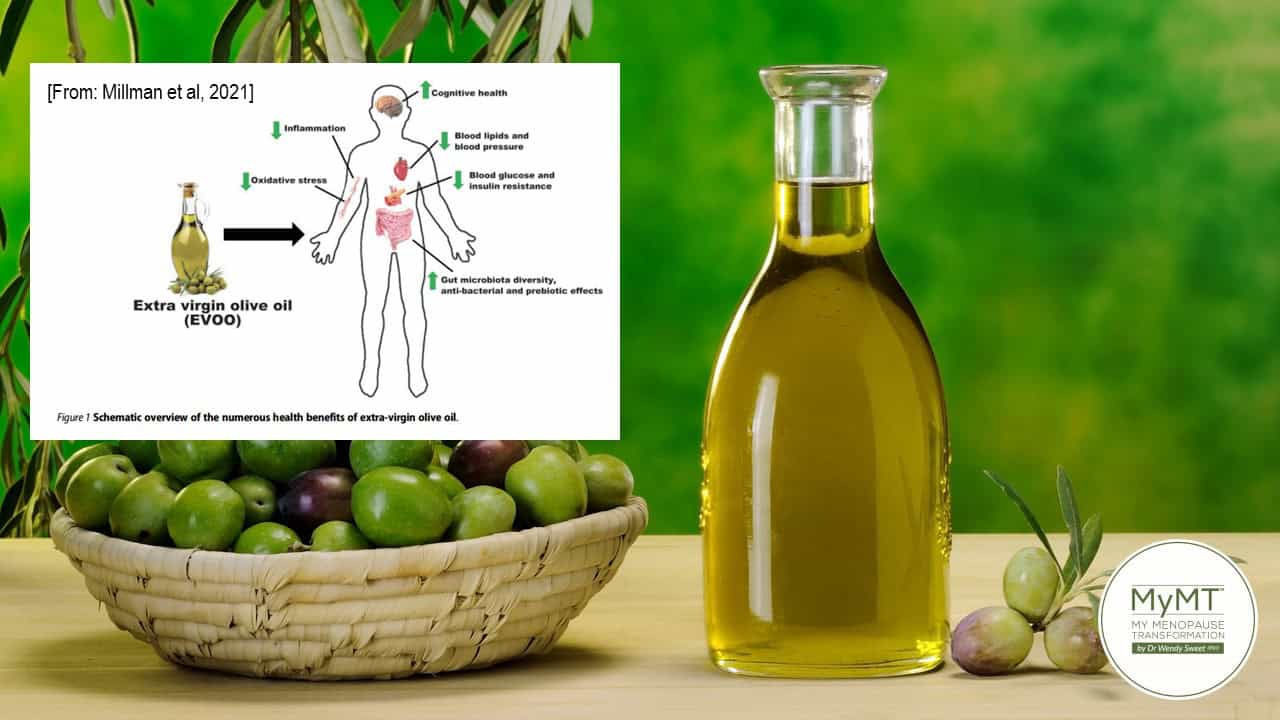
- Feed your brain the healthy Mediterranean Diet, including Extra Virgin Olive Oil –This is the approach I take in the MyMT™ programmes, however, I’ve modified the Med Diet specifically for menopause and post-menopausal women. What we must remember however, is that the energy demands of our brain is high. We need to ensure that we feed our brain. If women are thin and fasting a lot, but experiencing menopause brain fog and anxiety, then it’s important to reduce the fasting – your brain needs fuel!
Extra Virgin Olive Oil is also important to reduce your brain fog. Around 20 mls daily. It contains two compounds, oleuropein and hydroxytyrosol. Both these compounds have been shown to cross the blood-brain barrier, allowing them to directly exert their effects within the central nervous system, helping to reduce inflammation and brain fog. Furthermore, oleuropein binds to oestrogen receptors in the brain acting to help nerve pathways function more effectively. [Malliou, 2023].

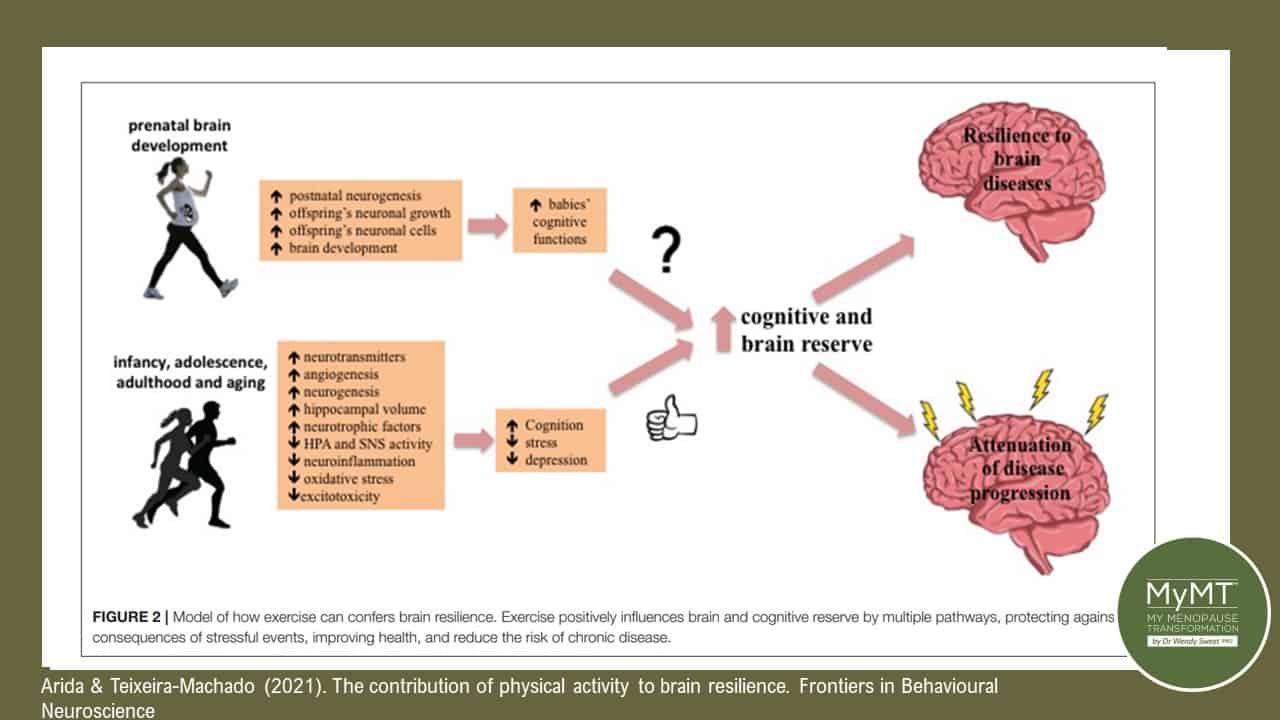
- Exercise aerobically – oxygen is stored in mitochondrial cells, hence your brain mitochondria require a lot of oxygen. Exercising aerobically, whereby you aren’t completely out of breath, helps your brain health. How we develop more mitochondria and improve their function as we age, is through daily aerobic exercise.
- Exercise and Mindfulness help to boost glutamate production in the brain. 80% of all nerves in the brain need glutamate in order to transmit nerve impulses but chronic stress negatively impacts glutamate production. Glutamate is important to memory, cognition, and mood regulation and both exercise and mindfulness have a strong impact on brain glutamate levels. (Pal, 2021).
- Reduce or remove alcohol. “The effects of alcohol last in the brain for up to several weeks” mentioned Sarnyai in his presentation. If individuals are experiencing changing moods, depression or increased anxiety, then it’s important to reduce or remove alcohol. Put simply, alcohol damages brain mitochondria.
- Stay connected … social isolation affects brain mitochondrial health but positive social interaction helps to buffer stress.

Understanding Mitochondrial Dysfunction in Menopause Brain Fog
Menopause hormonal changes, stress, poor nutrition, and ageing, disrupt mitochondria’s many functions.
This is why longevity and health researchers are finding that when it comes to our metabolism, energy production, immune health repair and regeneration, our tiny mitochondria matter more than we think.
Mitochondrial dysfunction appears in a wide range of brain and other health disorders and during menopause, mitochondrial dysfunction can accelerate.
Over the last decade, accumulating evidence has suggested a causative link between mitochondrial dysfunction and ageing and yes, declining levels of oestrogen has a role to play in this. [Henderson & Brinton, 2010; Lejri et al, 2018;
Whilst millions of women find relief from their menopause brain fog and mood swings with oestrogen replacement medications and/or anti-depressants, and whilst there seems to be a window of opportunity in peri menopause to take Menopause-HRT, making changes to our lifestyle to help maintain healthy mitochondria is important, as Professor Sarnyai reminds us as well.
Numerous changes occur around the body during and after menopause. These changes are perfectly normal … until they aren’t and start to impact your quality of life.
That’s the purpose of the 12 week programmes that I’ve designed for you. I hope you can join me on whichever programme suits you, or start easy with my Masterclass on Menopause webinar. I tell you about it in the video below.
Dr Wendy Sweet (PhD)/ Member: Australasian Society of Lifestyle Medicine
References:
Arida RM, Teixeira-Machado L. The Contribution of Physical Exercise to Brain Resilience. Front Behav Neurosci. 2021 Jan 20;14:626769. doi: 10.3389/fnbeh.2020.626769.
Bennett, S. (2016). Mighty Mito: Power up your mitochondria. Amazon Books: Santa Monica: USA
Berger M., Juster RP., Sarnyai Z. (2015). Mental health consequences of stress and trauma: allostatic load markers for practice and policy with a focus on Indigenous health. Australas Psychiatry. 23(6):644-9. doi: 10.1177/1039856215608281.
Eyre HA, Lundin R, Falcão VP, Berk M, Hawrot T, Leboyer M, Destrebecq F, Sarnyai Z, Reynolds C 3rd, Lavretsky H, Kolappa K, Cummings J. Brain Health Is a Determinant of Mental Health. Am J Geriatr Psychiatry. 2023 May; 31(5):379-381. doi: 10.1016/j.jagp.2023.02.005.
Filler, K., Lyon, D., Bennett, J., McCain, N., Elswick, R., Lukkahatai, N., & Saligan, L. N. (2014). Association of Mitochondrial Dysfunction and Fatigue: A Review of the Literature. BBA clinical, 1, 12–23. https://doi.org/10.1016/j.bbacli.2014.04.001
Henderson, V. W., & Brinton, R. D. (2010). Menopause and mitochondria: windows into estrogen effects on Alzheimer’s disease risk and therapy. Progress in brain research, 182, 77–96. https://doi.org/10.1016/S0079-6123(10)82003-5
Kwon, D. (2021). Could Mitochondria Be the Key to a Healthy Brain? Scientific American. Publ. June 18th, 2021.
Lejri, I., Grimm, A., & Eckert, A. (2018). Mitochondria, Estrogen and Female Brain Aging. Frontiers in aging neuroscience, 10, 124. https://doi.org/10.3389/fnagi.2018.00124
Malliou, F., Andriopoulou, C. E., Kofinas, A., Katsogridaki, A., Leondaritis, G., Gonzalez, F. J., Michaelidis, T. M., Darsinou, M., Skaltsounis, L. A., & Konstandi, M. (2023). Oleuropein Promotes Neural Plasticity and Neuroprotection via PPARα-Dependent and Independent Pathways. Biomedicines, 11(8), 2250.
Melhuish Beaupre LM, Brown GM, Braganza NA, Kennedy JL, Gonçalves VF. (2022). Mitochondria’s role in sleep: Novel insights from sleep deprivation and restriction studies. World J Biol Psychiatry. 23(1):1-13.
Micheli, L., Bertini, L., Bonato, A., Villanova, N., Caruso, C., Caruso, M., Bernini, R., & Tirone, F. (2023). Role of Hydroxytyrosol and Oleuropein in the Prevention of Aging and Related Disorders: Focus on Neurodegeneration, Skeletal Muscle Dysfunction and Gut Microbiota. Nutrients, 15(7), 1767. https://doi.org/10.3390/nu15071767
Menopause Brain Fog: Frequently Asked Questions
Menopause brain fog refers to cognitive symptoms such as memory lapses, forgetfulness, and mental fatigue that occur during menopause. These symptoms are often caused by hormonal shifts and changes in mitochondrial function in the brain.
Yes, many women experience brain fog in peri menopause due to fluctuating hormone levels and stress-related impacts on brain mitochondria. This often presents as reduced concentration, forgetfulness, and mood changes.
Menopause-related brain fog can be caused by declining estrogen levels, stress, lack of sleep, poor nutrition, and mitochondrial dysfunction, all of which affect cognitive performance.
Yes, managing stress, eating a Mediterranean-style diet, staying socially connected, getting regular aerobic exercise, and avoiding alcohol can all help reduce menopause brain fog.
For some women, estrogen therapy may help relieve brain fog. However, lifestyle strategies to support mitochondrial health are also highly effective, especially during peri menopause.