I remember the conference in New York distinctly.
It was 1995, the year my daughter was born. As it’s her birthday this week, I was remembering that trip as it was my first time away from her. However, attending the conference was an opportunity that I didn’t want to miss. I was presenting at an American health and exercise conference and for the first time ever, there were specialist presentations on medical concerns associated with exercise prescription.
Sitting in one of these sessions, it was the first time that I had heard a name given to the cocktail of conditions that I was seeing in overweight middle-aged women coming into the gym. When taking their physical and healthy history as part of their pre-screening, many of them described abdominal and breast weight gain, high blood pressure, pre-diabetes (insulin resistance) and high cholesterol.
Here I was, for the first time ever, hearing that these conditions were collectively known as Metabolic Syndrome [MetS], or as it is more popularly known, Syndrome X.
Nearly 30 years later, I continue to remember this conference … because as I went into menopause, the same health changes happened to me.
The menopause transition is now known to be a catalyst for the development of Metabolic Syndrome and a condition called Insulin Resistance. [Mumusoglu & Yildiz, 2019]. Of concern for all of us, is that MetS precedes Type 2 Diabetes as well as an increasing risk of cardiovascular changes as we age.
With an eye on our future health as we navigate menopause, the management of insulin and blood sugar levels is one of the hallmarks of managing metabolic syndrome and therefore, your changing weight during your menopause transition.
If you are overweight or obese, tired, feeling sluggish, have developed foggy brain, aching muscles and perhaps you always feel grumpy, then please don’t necessarily blame your changing hormones in menopause – blame your changing insulin and glucose metabolism as well as the changes to your muscles.
If any of these symptoms sound familiar, then please read on. Obesity superimposed on menopause and our ageing, drastically increases chronic low-grade inflammation (a condition called ‘inflammaging’ which I’ve written about in the past), and inflammaging is now seen as an important link between obesity, insulin resistance, and age-associated diseases. [Frasca et al, 2017].
I want you to understand the role of insulin and why it is so crucial to manage the secretion of insulin from our ageing pancreas in response to blood sugar levels. With better control of insulin release from our pancreas, we help to control our energy levels, moods, hot flushes and our weight.
Menopause can lead to changing insulin production and secretion. This is primarily due to the ageing of our pancreas. In turn, inflammatory changes in the pancreas may lead to unstable insulin production leading to high levels of glucose in the blood. Whether women are overweight or not, this can lead to Type 2 diabetes.
That’s why, if you aren’t sure about your glucose levels, then the next time you get your bloods checked, make sure that you get your HbA1c blood test done (as well as your triglycerides and your cholesterol levels). HbA1c is a diabetes test and measures your average plasma glucose concentration.
What does Insulin do in the body?
To better understand insulin resistance, it helps to have an understanding of the two hormones that are released by your pancreas when we eat.
These two hormones, insulin and glucagon, interact to help manage our blood sugar levels or blood glucose levels. If both these hormones are out of balance, our blood sugar/glucose levels become unstable.
This can lead to energy peaks and dips throughout the day, worsening mood swings and unstable weight gain.
Our pancreas manages Insulin production and release in response to blood sugar levels.
If you’ve eaten something really sweet or highly processed carbohydrates, then your glucose levels in your blood increase. To manage these higher blood sugar levels and remove them, insulin is released.
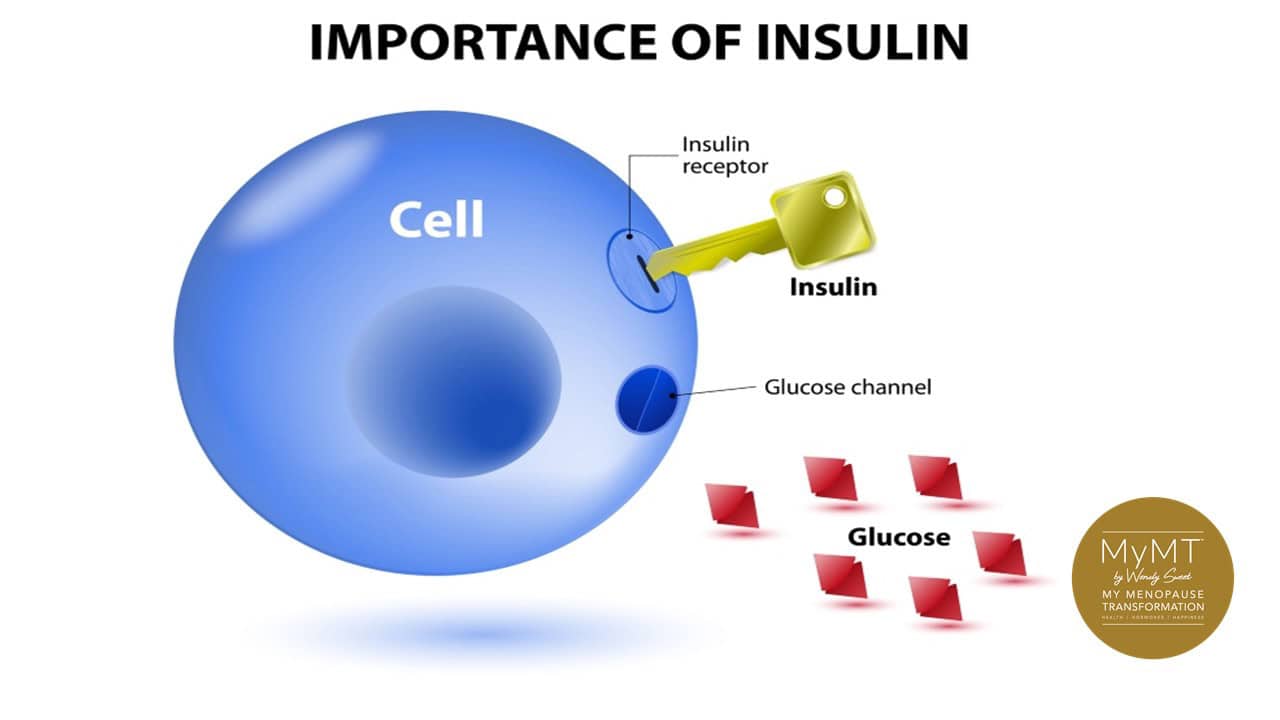
The normal role of insulin is to carry sugar or glucose to nearly every cell around your body. This includes your brain, muscle and liver cells.
Insulin carries sugar/glucose. It is your energy storage hormone.
When you eat something such as white bread or white rice, or a cookie or honey, your blood glucose (sugar) rises. This signals the pancreas to release an amount of insulin necessary to carry the available glucose to the brain, the liver and muscles as well as other cells.
There is no energy storage in our muscles or liver cells without insulin. Nor is there glucose which travels to the brain without insulin. It is a crucial hormone which holds the key to unlocking the door to glucose being stored in the liver, muscles and in fat cells.
In normal situations, insulin moves glucose into our brain, muscle and liver cells ready to supply energy for activity and metabolism. Sometimes however, this process gets out of order. This may be from:
- eating the wrong types of food,
- eating too much or too little food,
- drinking a lot of alcohol,
- having a sedentary lifestyle with very little activity,
- having too much exercise/sports as with athletes training and competing,
- carrying too much body-fat,
- the ageing of our pancreas during menopause, which is the organ responsible for releasing insulin and glucagon (it’s opposing hormone).
- the ageing of our muscles and liver (this reduces the efficiency of glucose storage into cells)
All of these factors can cause the pancreas and the liver to become inflamed and therefore, cause our blood sugar levels to get out of balance, either going too high, or too low.
When blood sugar levels are too high, the ageing pancreas works harder than ever to release insulin. If insulin is released too rapidly or too regularly, in response to increased blood sugar levels, then our cells and tissues can’t cope. Nor can we.
Hot flushes may become worse (because insulin helps to regulate temperature), and with the swings and dips in our blood sugar levels, just like hungry children, our moods can also change quickly.
Why too much Insulin is a potential problem in menopause.
Too much glucose in the blood can be problematic to women during menopause, because insulin also carries it to fat cells too.
Insulin regulates the uptake of dietary fats and glucose from simple carbohydrates into fat cells, especially if we have a large meal, or we are more sedentary (our liver and muscles use up glucose during exercise), or for women during menopause, if we aren’t sleeping.
For many women who have sore joints or are exhausted from not sleeping during their menopause transition, it’s very easy to become more sedentary. Especially if we have jobs and home arrangements that demand our time – this includes looking after ageing parents.
I understand how women feel – the worse my sleep was, the worse my joints and muscles felt, and I didn’t have the energy for exercising, nor did I have the time. My weight gain was also a hindrance to being able to enjoy more vigorous exercise.
However, not exercising or remaining active, as well as not sleeping well, may contribute to a condition called insulin-resistance.
The term ‘insulin-resistance’ comes from the knowledge that our cells can become resistant to insulin arriving to deposit glucose into them.
If women become insulin resistant, their liver, muscle and fat cells do not respond to the normal role of insulin properly.
This situation can build up over years due to a diet that is high in carbohydrates (especially processed carbs), but can also become accelerated in peri-menopause when oestrogen levels fall and inflammatory changes in cells occur. This includes in our pancreas and liver.
Insulin Resistance may lead to Metabolic Syndrome … just as I heard about back in 1995, when the Doctor presenting the session spoke about the changing cardiac and metabolic health of our mother’s generation in post-menopause.
As a young ’30-something’ year old at the time, I had no inkling that the same thing might happen to me. Many women who come on my programmes are the same.

When the cells do not respond to insulin, they don’t allow sugars from the blood stream to enter into them. So, the normal processes for insulin to be taken up by cells is ‘blunted’. This is the what causes ‘insulin-resistance’ which can occur on it’s own, but is always included in Syndrome X, or Metabolic Syndrome.
The key underpinning of Syndrome X is insulin resistance.
When cells don’t allow insulin to do its job, sugars from the foods you eat, including carbohydrates, as well as sugar released from the liver, build up in your blood-stream.
Sugar [glucose] in the bloodstream sends a signal to the pancreas to step up its insulin production in an attempt to maintain a normal blood sugar level. But because the liver, muscle and fat cells are resistant to insulin doing its job, the result is a by-pass of the normal processes and the sugar moves directly to fat cells.
In menopausal women, glucose may then move into storage areas under the diaphragm and into the stomach regions.

Manage Insulin Resistance with my 3 tips:
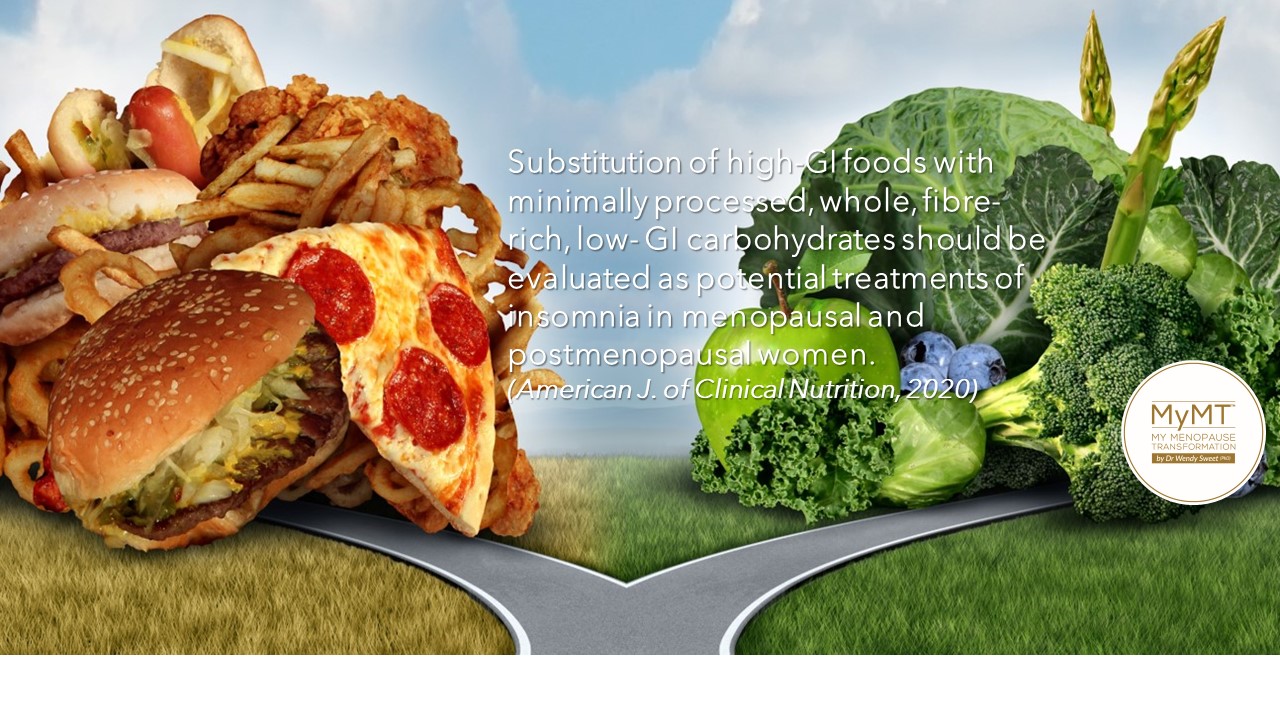
- Know that nutrition and adherence to it, is your best medicine. As such, you need to understand that the evidence behind the Mediterranean Diet for women in menopause to manage weight has been evolving for years. This is the type of dietary approach that I take in the MyMT™ programmes and have modified this to suit menopausal and post-menopausal women.

- Go for (mainly) low glycemic index carbohydrates. If you have been following my newsletters for a while, then you will have heard me discuss the low glycemic index. Pioneered by Professor Jenny Brand-Miller from Australia, this rating scale helps us to find carbohydrates that don’t spike insulin levels. I have lists in your MyMT™ programme all ready and waiting for you.
3. Improve Joint Health so you can move more freely and get active again. Did you know that your joints have oestrogen receptors in them? That means when we move through menopause, the reduction of oestrogen affects our joints. So too, does the slower turnover of collagen.
If your joints are aching and preventing you from being active, then you are more at risk of developing insulin resistance and/or metabolic syndrome.
I have more information in my Joint Health module within my 12 week programmes. In this powerful module, you will discover that there is a nutrient found in olive oil that replaces the loss of oestrogen in our tendons. This is why changing our nutrition to meet the specific changes that occur during menopause is so important to put into action.
When we begin to develop health changes in our menopause and post-menopause years, it’s hard to remember that we can turn this around and feel great again.
It’s the same with insulin resistance – you can reduce and reverse insulin resistance and/or metabolic syndrome.
If you don’t get on top of managing insulin levels then not only do you acquire more inflammation and gain more weight, but metabolic changes may arise too.
If you aren’t sure what to do, and/or if you are busy and want to feel supported then I invite you to join me on the 12 week MyMT™ Transform Me weight loss programme when you can. I hope you can join me on my January New Year, Healthier You’ promotion HERE.
Dr Wendy Sweet (PhD) Member: Australasian Society of Lifestyle Medicine.

References:
Carr MC. The emergence of the metabolic syndrome with menopause. J Clin Endocrinol Metab. 2003 Jun;88(6):2404-11.
Frasca D, Blomberg BB, Paganelli R. Aging, Obesity, and Inflammatory Age-Related Diseases. Front Immunol. 2017 Dec 7;8:1745.
Godoy-Matos AF, Silva Júnior WS, Valerio CM. NAFLD as a continuum: from obesity to metabolic syndrome and diabetes. Diabetol Metab Syndr. 2020 Jul 14;12:60.
Ko SH, Kim HS. Menopause-Associated Lipid Metabolic Disorders and Foods Beneficial for Postmenopausal Women. Nutrients. 2020 Jan 13;12(1):202.
Manco, M. ,Nolfe, G. , Calvani, M., Natali, A., Nolan, J., Ferrannini, E., Mingrone, G. (2006). Menopause, insulin resistance and risk factors for cardiovascular disease. Menopause, 13 (5), 809-817
Martín-Peláez, S., Fito, M., & Castaner, O. (2020). Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients, 12(8), 2236. https://doi.org/10.3390/nu12082236
Minu S. Thomas, Christopher N. Blesso, Mariana C. Calle, Ock K. Chun, Michael Puglisi, and Maria Luz Fernandez. Dietary Influences on Gut Microbiota with a Focus on Metabolic Syndrome. Metabolic Syndrome and Related Disorders.Oct 2022.429-439.
Mumusoglu S, Yildiz BO. Metabolic Syndrome During Menopause. Curr Vasc Pharmacol. 2019;17(6):595-603.
Patni, R., & Mahajan, A. (2018). The metabolic syndrome and menopause. Journal of Mid-life Health, 9(3), 111–112.
Stachowiak G, Pertyński T, Pertyńska-Marczewska M. Metabolic disorders in menopause. Prz Menopauzalny. 2015 Mar;14(1):59-64. doi: 10.5114/pm.2015.50000.
Wang, Q., Ferreira, D.L.S., Nelson, S.M. et al. Metabolic characterization of menopause: cross-sectional and longitudinal evidence. BMC Med 16, 17 (2018). https://doi.org/10.1186/s12916-018-1008-8
Weickert M. O. (2012). Nutritional modulation of insulin resistance. Scientifica, 2012, 424780.